Hypoxic Ischemic Encephalopathy, or H.I.E., occurs when blood flow and oxygen are restricted to the brain.
Thankfully, there are patient advocacy organizations with game-changing leadership, Hope for HIE, to guide parents through their journey.
Families whose new baby has been given this diagnosis face more questions than answers, starting with when the H.I.E. officially has happened. While it can occur during childbirth or pregnancy, there can be many causes of H.I.E. The diagnosis varies wildly which is another source of stress for families – no two cases are exactly alike.
The treatment for babies that meet a certain set of criteria is therapeutic hypothermia – this means the baby’s body temperature is lowered in a controlled environment. The reason doctors initiate this treatment is that it decreases. the risk of mortality, moderate-to-severe disability, cerebral palsy, visual deficits, cognitive delays, and psychomotor delays. (Allen & Brandon, 2011). The cooling cap and blanket circulate water that is initially cold and then warmed after 72 hours.
What to Expect during Therapeutic Hypothermia
Understanding how treatment works is essential to feeling that parents are active participant in their baby’s care in the NICU. During therapeutic hypothermia treatment, you can expect the following according to Sakr and Balasundaram (2022):
- A cooling cap or blanket will be used to lower the body temperature to 92.35 degrees fahrenheit and keep it the same temperature for 72 hours.
- The baby is intubated with a breathing tube to make sure their airway is cleared and a central line is placed usually in the baby’s belly button through their umbilical artery to be able to administer medications and fluids as needed.
- Their blood pressure, pulse, cardiorespiratory rate and EKG is set up to continuously monitor the baby during the cooling process to ensure they are tolerating it well.
- Labs are also taken to measure electrolytes, glucose, creatine, among others and the input-output from the baby is monitored through a foley catheter to measure the effects of the cooling treatment.
How to Promote Bonding
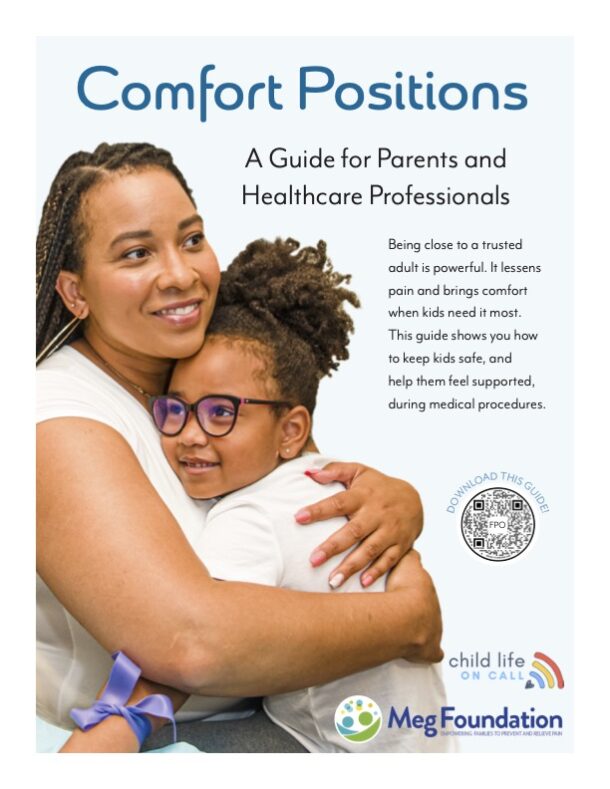
Knowing that baby will have wires and numerous body functions being monitored can be really scary to see – much less to know how to physically interact. After nine months of parents waiting for the moment to hold their baby, waiting those extra days can feel frustrating and upsetting.
It is a natural instinct for parents to want to hold their baby, take their pain away, and comfort them.
So, when their baby can’t be held, it’s essential for child life specialists to concretely and efficiently communicate ways for parents to bond with their baby.
— Katie Taylor, CCLS (@childlifeoncall) April 17, 2023
Here are a few suggestions for bonding, but make sure you always talk with the primary neonatologist to make certain that baby can tolerate certain activities such as being read to, talked to, hand held, etc. as it’s possible that even the smallest bit of stimuli could be painful after a brain injury like H.I.E.
Hope for HIE families can receive 1:1 child life specialist support here.
In recent years, holding during therapeutic hypothermia is becoming more accepted and used by professionals. Always advocate for bonding by asking your doctor as well as for Child Life to come to support bonding through various interventions. Some ways to promote bonding include:
- Softly singing
- Quietly reading a book to them, preferably one that was read to them during pregnancy
- Talking to baby, softly saying you love them, telling them about their family, what your want to experience with them and about the future
- Advocate to hold baby. 100% of mothers said they believed other parents would benefit from holding their baby during therapeutic treatment and 75% of nurses strongly agreed that after completing 30 minutes of holding with close supervision and monitoring, it was safe (Craig et al., 2019).
- Advocate for your involvement in routine care such as diaper changes, dressing changes, washing, etc. and being there when these things take place
- Hold your infant’s hand and have them feel your presence
- Ask to see a lactation consultant to help you be able to pump if you wish to breastfeed. Continuing with pumping will allow your baby to receive your breast milk when they are cleared to begin feeds, it could also allow you to still be able to breastfeed in the future.
For Professionals
As professionals, we have to recognize the trauma and loss of normalcy caused by these experiences. Parents deserve to be involved in their child’s care and need to be communicated with in excess as they process the events from birth until now. When talking to parents, remember they are scared, exhausted, and experiencing a traumatic event. To facilitate communication and a positive relationship with parents, try these tips:
- Instead of asking “Do you have any questions?”, ask “What questions do you have for me?”. By changing this wording, it acknowledges the parent’s natural need for information. Encourage parents to write down questions they think for future meetings.
- Show compassion by listening attentively and calmly answering parents’ questions. Parents reported they felt comforted knowing there was a human being behind the professional role (Wigert et al., 2014).
- Make small talk to allow the parents to be more than a parent with a sick child and recognize there is a life outside of the NICU.
- Recognize the milestones and celebrate the progress no matter how small. By only coming unannounced when there’s bad news, parents reported feeling a sense of imminent danger when the doctor came in and often felt they were rushed and did not have an opportunity to discuss what the bad news meant for their child and that news was delivered in passing (Wigert et al., 2014). By celebrating the milestones and small progress, parents will not associate visits as exclusively negative.
By taking the time to communicate with parents, it helps them feel included in their child’s care by feeling heard, understood, and informed. Parents need to be supported by providers and professionals through reminders to eat, get sleep, and be provided updates on their baby when they aren’t there, really focusing on the positives. Understanding the parental bond and drive to comfort and fix is so important as parental mental health is strained during this time.
By promoting bonding, we can provide some normal experiences many parents who experienced a traumatic birth, scary diagnosis, and time in the NICU miss out on. This can be an isolating time for many parents so social workers and child life should be knowledgeable of resources and support for these parents as they navigate this challenging time. When implementing a few changes in your approach and care of children and parents affected by H.I.E., you are going beyond the physical needs of the child and addressing the emotional needs of both the child and the parents, strengthening provider- parent communication and relationships for a more effective care team.
For more information on H.I.E. check out Hope for H.I.E. and Betsy’s Story on the Child Life on Call Podcast to hear from a parent of a child diagnosed with H.I.E.
References
Allen, K. A., & Brandon, D. H. (2011). Hypoxic Ischemic Encephalopathy: Pathophysiology and Experimental Treatments. Newborn and infant nursing reviews : NAINR, 11(3), 125–133. https://doi.org/10.1053/j.nainr.2011.07.004
Body cooling treatment. Texas Children’s Hospital. (n.d.). Retrieved October 14, 2022, from https://www.texaschildrens.org/body-cooling-treatment
Craig, A., Deerwester, K., Fox, L., Jacobs, J. and Evans, S. (2019), Maternal holding during therapeutic hypothermia for infants with neonatal encephalopathy is feasible. Acta Paediatr, 108: 1597-1602. https://doi.org/10.1111/apa.14743
Neonatal therapeutic hypothermia. Nationwide Children’s Hospital. (n.d.). Retrieved October 14, 2022, from https://www.nationwidechildrens.org/specialties/neonatology/our-programs/neonatal-therapeutic-hypothermia
Sakr M, Balasundaram P. Neonatal Therapeutic Hypothermia. [Updated 2022 Jan 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK567714/
Society, C. P. (n.d.). Hypothermia for newborns with hypoxic-ischemic encephalopathy: Canadian Paediatric Society. Hypothermia for newborns with hypoxic-ischemic encephalopathy | Canadian Paediatric Society. Retrieved October 14, 2022, from https://cps.ca/en/documents/position/hypothermia-for-newborns
Therapeutic hypothermia. Riley Children’s Health. (n.d.). Retrieved October 14, 2022, from https://www.rileychildrens.org/health-info/therapeutic-hypothermia
Wigert, H., Dellenmark Blom, M., & Bry, K. (2014). Parents’ experiences of communication with neonatal intensive-care unit staff: an interview study. BMC pediatrics, 14, 304. https://doi.org/10.1186/s12887-014-0304-5