Today’s guest is Erin Prosser, an IEP expert consultant and a mom of a daughter diagnosed with STXBP1. "You don't see it coming. Being a rare disease parent hits you like a ton of bricks." In today's episode Katie Taylor had the chance to speak with Erin Prosser, an...
Episode 177 | Kimberly’s Story – Cord Prolapse and Emergent C-Section at 26 Weeks
Podcast Show Notes
Finding Support in the NICU: Kimberly Reyes Discusses Building a Parental Community
In this episode of the Child Life On Call podcast, NICU mother Kimberly Reyes shares her emotional journey of advocating for her premature daughter’s care. With healthcare professionals disregarding her wishes and COVID-19 regulations separating her from her baby, Reyes’ story ends abruptly, leaving listeners wondering: will she be able to take control of her daughter’s care and beat the odds?
You try to hold on to the slightest bit of control because it is a situation where all control over your own body, the process, your child, everything is kind of taken away from you.
My special guest is Kimberly Reyes.
We are excited to introduce Kimberly Reyes, a compassionate mother who channeled her own NICU journey into a mission to inspire and educate other parents. With a background in teaching that spans 15 years, Kimberly has a natural ability to connect with others and share her story in an impactful way. Facing the challenges of having a premature baby during the global Covid-19 pandemic, she has become a resilient advocate for parental involvement in the NICU. Kimberly’s firsthand experience of fighting for her child’s care and advocating for her family has made her story both relatable and inspiring for other NICU parents.
This is Kimberly Reyes’s story:
The world of the NICU was a new and challenging terrain for Kimberly Reyes, who found herself grappling with a premature newborn at just 26 weeks. A former teacher and passionate mother, Kimberly quickly realized the importance of standing up and advocating for her daughter’s unique needs amidst the hustle and bustle of a massive hospital. Through her tireless persistence, she made certain that her baby received the comfort and care she deserved, even going as far as hand-expressing colostrum and putting up bold, colorful signs to make her wishes known. Kimberly’s journey is a testament to the strength of a mother’s love and an inspiration to other parents traversing the same path, encouraging them to be vocal advocates for their children in the NICU.
In this episode, you will be able to:
- Unravel the art of parental advocacy and participation in a NICU setting.
- Probe into the emotional and psychological toll of having a child with complex medical needs.
- Discern the value of empathy in delivering exceptional patient-oriented healthcare.
- Understand the importance of flexibility and adaptability in the practices of healthcare professionals.
- Unearth innovative techniques to combat burnout and prioritize self-care among healthcare workers.
The resources mentioned in this episode are:
- Check out Kimberly’s LinkedIn page to see her creative writing style and advocacy work.
- Consider reading Kimberly’s future book or other writings about her NICU experience.
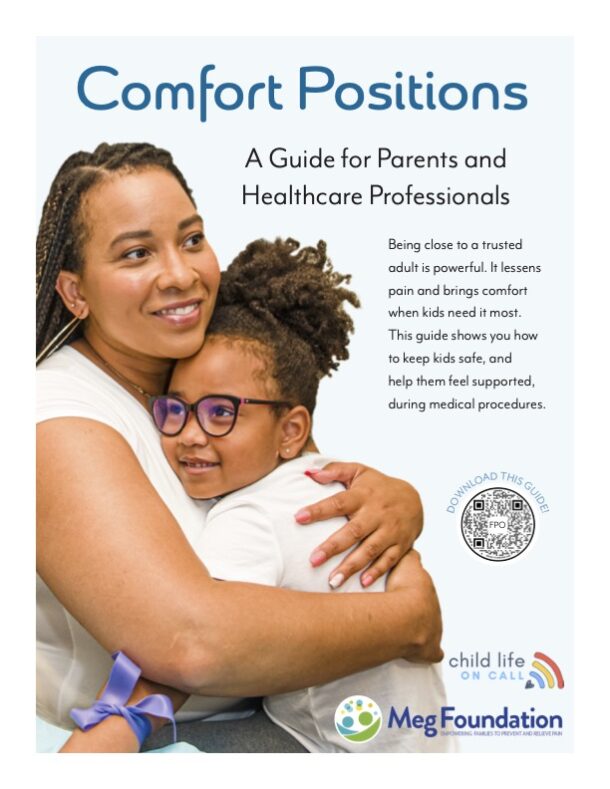
- Reflect on what matters most to you and your family before any medical emergencies or procedures.
- Advocate for yourself and your wishes during medical procedures and insist on what matters most to you.
- Support organizations like Child Life On Call provide support for families during medical emergencies.
Whether you are a parent or professional, we want you to join our community. Sign up for our newsletter here.
Parents, download our free parent starter kit.
When you download our starter kit, you’ll learn how to:
- Give medicine to your child without it becoming a wrestling match
- Prepare your child (and yourself) for a shot so they can feel less anxious
- Create and use a coping plan for any medical appointment or procedure
The first sign of sniffles, or worse, shouldn’t send you into a tailspin. Feel confident in your role as a parent and advocate, no matter what medical situation you’re facing.
Child life specialists, get affordable PDUs on-demand here.
Shop for your CLOC gear here.
Episode Transcript
00:00:02 It great. Well, if you don’t mind just kind of starting off by introducing us to who you are. Tell us your name, where you live, a little bit about your family, and a little bit just about your background. And do you go by Kim or Kimberley? What makes you the most comfortable?
00:00:19 Usually just Kimberley for professional purposes. Okay, Kimberley. Well, why don’t you introduce all of our listeners to who you are and a little bit about you and your family. Sure. So, my name is Kimberley Reyes, and I am a mother to a newly three year old.
00:00:36 So we hit three two weeks ago. Quite the journey. And so I live in western Montana now, in the mountains in rural Western Montana, although we are originally from New York City. So it has been quite different, quite the culture adjustment, but in all intentionality. And so I’ve got a kid that loves tractor poles and skipping rocks in the river, and it is just a different life.
00:01:08 That same child was born at 26 weeks, weighing one pound 8oz, and she spent 109 days in the NICU before she came home. And so that has shaped our parenthood and shaped our journey. And that’s kind of a little bit about who I am and we are. Wow. I have so many questions for you, and one is just to kind of give the listeners and ideas that you and I connected on LinkedIn, and I was immediately drawn to your ability.
00:01:45 I don’t know. It’s such a mix of I would say creative writing is your style. You speak to people like I can hear your voice through your words. I don’t know what that’s called, but just immediately gravitated to who you are, what you are willing to speak about, and the courage that it takes to speak about your own personal experiences and move into a professional vision. So I’m excited to get to what you’re doing now and how you’re advocating for yourself and for other families.
00:02:22 Sure. Walk us through kind of just back at the beginning and finding out that you were pregnant and was there any clue that you were going to have a preterm birth, or was it a surprise? Well, it’s one of those things that actually, having done more research, I wish I knew what I knew then. Now, actually. So I guess I’ll preface it.
00:02:42 So it’s interesting that you say the style in which I explain. I’ll preface also that I was a teacher for 15 years before my daughter was born. There it is. Yeah. We are used to standing in front of groups of people, talking about yourself, because if you aren’t personally involved in what you’re doing, kids tune out, adults tune out.
00:03:07 And so that’s, I think, a part of just the comfort with generally just talking to people. It’s something I did 6 hours a day, every day for 15 years. Well, I guess so. When I was first pregnant, which I suppose I guess was the fall of 2019 at about nine weeks. I had something called an Sch, which is a subcronic hematoma, and at the time actually thought it was a miscarriage.
00:03:36 Turned out it was just a bleed. Went to the hospital and an emergency room experience, which that’s a much longer story for a different day, but already started to in that experience itself, feeling some of that not being heard, not being seen, not being taken care of. And so fast forward to them saying everything will be fine. Had to find a new doctor because the gynecologist at the time wasn’t an OB. So it was just, okay, you’re pregnant, but you have to go see someone else.
00:04:13 So this was the first of four different providers I would actually have over the course of being pregnant, much more than four because if anyone’s been in the hospital, you know that you see a new doctor every 72 years. As far as families are concerned, there’s not a staffing shortage because there’s so many new faces every day. And I was in one of the nation’s premier teaching hospitals, so I’ll tell you, just the size of staff and turnover. But anyways, I was put on bedrest for a week and then I was told that once it sort of resolved itself, everything would be fine. Further research as a researcher and diving deep into medical journals myself, turns out had I maybe been on bed rest, things might have been different.
00:05:05 Because I really should not have gone back to the stress of teaching elementary school, being on my feet all day, being yelled at my parents, all of the different things that one deals with. But fast forward. So we were told at around 20 weeks everything was fine, that the original issue had cleared. She was developing well all of the sort of, okay, we’re in the clear now moments. Somewhere around then, I was actually fired by that OB.
00:05:36 That’s a thing that can happen. So people are always like, Wait, what? And I’m like, yeah, no, they’ll hand you your file in the lobby and tell you it’s been fun, but we’re not going to continue to do this. So at which point frantically searching happened through my pregnancy for another provider, I ended up going the midwife route and found for the first time someone who wanted to listen to the story and wanted to respect our wishes. And my husband and I left the appointment both looking at each other and saying, did someone just tell us that this is our kid and we have a voice?
00:06:11 Because that was refreshing and huge, but that would last for about two weeks. And about 23 weeks I was pre prom and my water broke, and I went in the hospital and all hopes of anything being not medicalized and natural and with wishes as I’d like, went out the proverbial window. And so at the time, when I was admitted, my daughter weighed only about 480 grams, I think they said, and was still a week under what they call Viability. So I was told if she were to come at that time, there would have been nothing they could do. And my job was to stay pregnant as long as humanly possible and get her weight up.
00:06:55 So I proceeded to lie there in the hospital and eat balls of buffalo mozzarell, a couple of other very high edible fat things, and she came at 26 weeks and four days weighing 680 grams. So she had gained those 200 grams. That’s impressive. Yeah. That’s amazing.
00:07:16 It is not easy to be on bed rest. No. And even the coat I wore into the hospital, I couldn’t wear home.
00:07:27 That is hilarious. Participated in said waking. But.
00:07:35 Can you eat buffalo mozzarella anymore, or does it take you back to that time? Well, I live in now what we call a food desert. So if I could get good Italian deli, I also spent two years living in Italy, so I’m a little bit spoiled with the whole situation. But if I could get real and good cheese, I would probably eat it till the end of time. Still today.
00:07:54 Okay. Good to know. Yeah. Well, and also just cold cuts in general, which most people avoid when they’re pregnant. And so the day that my daughter actually did come, my mom still tells the story of getting a call from my husband, who we had still wanted to encapsulate the placenta at that time.
00:08:11 And so I go into I don’t even think you could call it labor because I had a cord prolapse, the cord delivered before the baby. Right. Seven minutes later, crash, C section, she was out. So one could call it labor, I don’t really know. But anyways, my mom gets this frantic call from my husband, and he goes, I need a cooler and subgenic salami.
00:08:31 And my mom goes, what?
00:08:36 For the baby? You’re making absolutely no sense. It would later, months later, be clarified that the cooler was for the placenta, which actually couldn’t be saved because it had turned necrotic, which nobody had figured out. And the salami was for me to have a sandwich finally after I woke up from, oh, my goodness, Kimberley. Did she deliver on both of those?
00:09:01 I don’t think she brought the cooler because in the end of the day, she had no idea what he was talking about because there’s a fridge in her room. So I’m just going to ignore this part. And they came to the hospital, and she would bring me a whole spread of cold cuts probably a week later when I first came home from the hospital. And they were fresh from an Italian deli, and delicious, but nonetheless. So my daughter comes at 26 weeks, weighing a pound and a half, and we begin this NICU journey in.
00:09:30 And also, simultaneously, the day that she’s born, new York locks down for COVID series of events that conflate into the perfect storm of a situation where my husband and I were never allowed in the NICU together. And so she was 108 days, no, 108 days old before we were ever together as a family.
00:10:00 My heart breaks for you for so many reasons. I was a Child Life On Call specialist in the NICU during the pandemic and got to see firsthand what that was like for parents. And I can only hope one day that maybe you are writing a book or that you will produce something in addition to these podcasts because your written word about that experience is so important, especially with your talents of being able to communicate. Can you talk to me about you talk a lot about advocating for yourself, for your daughter. What did that look like at the beginning?
00:10:43 And were you the best advocate right after she was born? Is it a role you grew into? Like, talk to me about that process of becoming a NICU mom. Sure, yeah. So I’m going to say me yelling for her best interest began literally the second I woke up from surgery.
00:11:04 And so I was set in recovery. And one of the things that I think NICU parents will tell you is you try to hold on to the slightest bit of control because it is a situation where all control over your own body, the process, your child, everything is kind of taken away from you. And that’s something that I really think is very important for staff to consider. Right? So that I wake up from emergency crash dissection where the last thing I remember is being wheeled through a labor and delivery ward on my knees with a doctor behind me holding the cord in this level of just insanity of the whole thing.
00:11:58 Me telling the anesthesiologist, oh, well, can I move my arm here to help you out? Because I’m trying to help you out, because me panicking I know is not going to help. So how do I help? And he goes, well, actually, you can hold it there. So I said, okay, let’s do this together because we’re all here for the same thing.
00:12:13 You’re like, your success is my success. Teamwork is dreamwork here, people. Nonetheless, I wake up and I know that at that moment I’m producing colostrum. I’m producing the most nutritious thing humanly possible for a child who’s come early and this is what she needs. And so I say to the nurse, okay, I need a receptacle to hand express this colostrum.
00:12:40 And somehow somebody gets it to her. Oh, no, you rest, don’t worry about it, it’s okay. No, I’m not going to rest. You need to do this. Said nurse leaves.
00:12:52 Next person comes along may or may not have been an orderly, someone who had no excuse. You need to get me a cup for this collage. Okay, I’ll get a nurse. You do that. So I think it was probably three or four different people.
00:13:04 Me insisting in one can say not the least, I’m not the most polite person if you’ve decided not to respect my wishes. So saying this is what’s going to happen. And I was able to, after insistence, which I think many people wouldn’t feel the agency to do at that moment, right. Express the colostrum, my husband was able to take it downstairs and give it to her by mouth with a swab. Wow, that’s incredible.
00:13:37 But I think about it. I think about in that moment of just having to insist so deeply and my own conviction, my own sense of saying, no, this is what I want for her. And if I’m walking down there myself, I’m about to get out of this bed and do it. So someone needs to make it happen. But I think it shouldn’t be that hard, right?
00:14:05 Yeah.
00:14:11 I can’t say for certain. I don’t spend time with mothers right after they give birth. We typically see them once they get to the NICU. The picture that is painted for me is a parent who is scared, who is fearful, and every instinct is telling them, my baby should be with me right now, and they’re not. So how can we care teams, care providers, look at those little spots.
00:14:46 For you, it’s colostrum. For other people, it’s making sure data is there. For somebody else, it’s getting me off this pain medicine as soon as possible, whatever it is. That question should really be before the emergency, before the C section, before the birth, to say what is most important to you. I’m working with a hospital right now and they have this great line.
00:15:10 It’s called what matters most. And it’s like we take all the medical stuff out of the way, but what matters most to you and your family right now, we’re going to prioritize that and we’re going to put it in the chart that’s happening at Child Life On Call’s right now. And I think that’s so powerful. And all it would have taken is one of these people to look at you and say, what matters most to you right now? I’m going to listen.
00:15:31 I’m going to make it happen. Yeah, I mean, that’s mind blowingly amazing, first of all, to hear that someone is thinking in that realm, because I think one of the issues and so I’ll go back to the idea of the size of the hospital I was in and the size of the NICU and the fact that you’re talking about one of the nation’s premier teaching hospitals. So that there is on average, I think I do some quick math, 50, 60, 70 babies in the NICU. You’re not talking about a small operation and even the antipartum end of it. So when you deal with maternal fetal medicine before you give birth was a constant rotation.
00:16:17 I was there so long that I saw the rotation, like, come back twice. And I think, oh, hey, I haven’t seen you in a month. But nonetheless, I think it’s a moment where that bit of humanity because that’s really what it is. You’re talking about humanity, right? You’re talking about having the most human aspect of what a family needs being taken into consideration, right?
00:16:43 And I’ll give you an example of another thing. So when my daughter was, I don’t know, probably a few days old, the umbilical cord, the stub of the umbilical cord was still attached. And I come from a tradition where when that falls off, you put it in a little wax paper and it goes in the baby book. And mine, 40 years later, is still set in a baby book. That’s a thing.
00:17:07 And so I had left explicit instructions with anyone who would listen when it falls off, please save it, please, the nurse, the person changing limits, anybody who would listen for that first three or four days. And if my husband went in the morning when I didn’t go, I said, make sure you tell them that this is what’s going to happen. I show up, must have been day four or five, it’s gone, it’s fallen off. I noticed, not because I was able to change her diaper, but because I was there for cares and someone else was handling my child when I had never even held her, right? And I said, well, where’s the intelligent cord?
00:17:47 And I started to cry. At that point, I lost it because I said, I only asked for one thing, guys. They said, in the general scheme of things. And the nurse just looks at me and she goes, oh, well, it must have just fallen off in a diaper change and things happen and walks away. No?
00:18:10 Yeah. And I remember telling anyone who would hear, and each person that I spoke to was, it was met with the same sterility and lack of things. And I don’t think until there were, you know, tears falling down my face, that the one woman looked at me and said, I’m sorry. And I said, well, what does sorry do here? What does this change?
00:18:40 This is gone forever, this moment. And the fact that not only were the wishes not even respected, but there was such a flippancy with which the response was given as well. Needless to say, anything else that I had in the future, I stuck giant signs to the incubator. And I had our amazing childlike specialist at the hospital who helped me. She’s like, I can laminate those for you.
00:19:06 I was like, let’s do it. There are pictures of my daughter’s incubator with giant sides, laminated with bright colors of every little thing that we wanted someone to know so that if you walked over there, there was really going to be no way you were going to miss our wishes. I love a good sign. I’m not surprised that you did this. I’m so glad you did that because gosh, every family who comes into the hospital, okay, hear me out for just a quick second.
00:19:40 We’re going to dream is given ten pieces of cardstock and a big ass Sharpie. And it’s like the things you want, please put on the door your wishes, your this and that. Like, oh, goodness, my heart is breaking for your umbilical cord. I haven’t had a family ask for that. And my mom has my umbilical cord and wax paper in my baby book.
00:20:09 I’m sorry that you were met with that. I’m sorry that somebody was too scared to look at you and say, I’m so sorry. I cannot believe we’ve overlooked this. I know where the trash is. I know where we put the baby diapers.
00:20:26 I’m going to go in and look and you deserve that something. I think it was at a point where they were at some level glad to see us go because I started telling other Bobs, I’m like, hey, do you have a sign?
00:20:45 Can everybody have a sign? Do you want that? Just even things like them putting the first outfit on a baby. Because if anyone has been a NICU parent, you know that they don’t wear clothes for a long time. And so when you finally get to wear clothes, right, it’s a big deal.
00:21:02 And so I said, do not put that first outfit on her without me here. I will be the one to do this, right? And so just another thing that went. On the sign, did that happen and were your wishes met for that?
00:21:23 I came in one day and she was wearing I don’t know if you ever kind of looks like almost like a karate gee. It’s like the white robe that they put on the baby that has sort of two flaps in the front and it ties around the waist and it’s like the baby version of hospital thing. So I came in one morning and she’s wearing one of those and I’m like, what is this? Like clothes? And so had a moment about it and they said, oh, well, we just put this on.
00:21:53 I said, oh, well, that’s technically closed. Shall we have a debate about what is really close or not? Because we can place semantics. I’m a linguist. Let’s not do this.
00:22:04 Sure.
00:22:07 The actual clothes that a relative of us had sent us an entire Trusseau of premie stuff. So according to the staff, she was the most fashionable nicki baby they’d ever seen with just this ridiculous series of pajama after pajama. And so the actual outfit that was bought for her, I did eventually get to put on her for the first time. It’s these tiny touches that make you mom that we have to hold on to and celebrate and gosh, I wish I was a linguist. Right.
00:22:44 You right now, because I lose words facilitate for parents to have those moments. I think putting on the first outfit. Go ahead. I think deeper than that. Not only facilitate them, but be cognizant of the fact that that should never have had to be the case in the first place.
00:23:08 So I think there’s a disconnect because it seems to be in an attempt to be such good caregivers, right? And I’ve got love till the end of time for the NICU staff and for the people that did literally keep her alive, that’s that’s not the point. But to understand what it means for a parent, that all of that agency has been taken away. So that for someone to have to facilitate me holding her for the first time, which, by the way, didn’t happen until she was 57 days old, and me to wait that morning for a nurse to flippantly, say, okay, well, she’s been excavated, but you still have to wait 2 hours because it’s not care time. And I almost lost it.
00:23:58 What do you mean? I’m sitting here. We’ve been waiting until today was the day. This is holding day. And so, really, to deeply understand what it means psychologically for a parent to not be able to make those decisions, to not be able to pick up a child when they want, to not be able to nurse, to not be able to decide how much and at what time and by whom they’re being fed all of these things that are normally a given.
00:24:27 Right? As the parent. And so not even saying how do we facilitate it, but recognize what it means that you, as the staff and the provider and whatever position you hold now, have to facilitate something for someone, that it should just be that person doing it.
00:24:52 That’S really important. I think you’re right. I know you’re right.
00:25:00 It’s a recognition. And I think that’s when we talk about sort of the deepest levels of sympathy and in some cases empathy, empathy is hard because you have to have experienced it in order to understand. Right. Sympathy is a bit easier because you can say, I understand how you feel, as opposed to saying, I know how you feel. Right.
00:25:21 But just recognizing the grief. And what I love in a lot of the NICU community is we talk about different things, about grief. Grief is not just the loss. Grief is also looking at the loss of experience. And so understanding that parents with a child in the hospital are grieving so many things, and chief amongst which is they’re grieving normalcy.
00:25:55 They’re grieving having that picture perfect birth and holding the child after you birth it. And the Pampers commercial we’ve all seen, which I still can’t really handle, kind of brings tears to my eyes because I’m just like, that never happened.
00:26:12 And understanding what it really means to be dealing with a family that’s grieving the loss of expectation, the loss of normalcy, the loss of a joyous experience surrounding the birth of a child.
00:26:31 Kimberley what has helped you the most since having this very transformative experience of being thrust into the medical setting with you? Not just you, but you and your baby, your husband. But when we strip away the educator part of you, the historian part of you, what has helped the most for you and yourself, your personal journey through all of this? I think finding community, finding that, understanding that I’m not the only person who feels this way. And so there’s in the course of doing the podcast, in the course of doing the research I’ve done, I’ve connected with a lot of parents all over the world.
00:27:28 I had a great email exchange with someone in Australia this morning, and we’re trying to figure out a time for a phone call, and we’re like, 16 hours is a crazy time. That is a crazy time. I told her. I was like, I deeply understand. I spent five years living in Tokyo, so trying to talk to anybody in the States was always a challenge.
00:27:46 But just reading a post where a mom is like, I cried because someone sent me a baby shower invitation today. And you sat there, and you’re just like, It’s not just me. And that sense of, It’s not just me because it is, in the best of circumstances so easily, so easy to feel isolated. But given the way that all circumstances have been exacerbated in the last few years, it was actually deeply isolating. It wasn’t actually just feeling isolated.
00:28:25 You, in fact, were isolated, right? And for many parents, still the same. Right? For children with medically complex, for parents with medically complex children, this is a reality that so many of the normal milestones, so many of the moments in life happen in isolation and happen in this sense that I’m the only one going through this right now and at this time. And knowing that not to be true has been comforting, empowering, and also a motivation to make sure that the next person feels that way, too, right?
00:29:08 So beautifully said. And I’m grateful that you’re doing what you’re doing now and sharing what you’ve been through. Where can people listen to your podcast, hear more from you, connect from you? And what kind of people do you want tuning in and following along with what you’re doing?
00:29:32 So we have a website. So the umbrella organization of everything we do is called all the Unexpected. I love that it came from a play on the what to expect, right? Because when you’re expecting a child, they tell you. And I sat there with the app, too, and I’m going, oh, we’re a grapefruit today, okay?
00:29:56 Doing all of these things, right? But what happens when it’s unexpected? What happens when the baby comes early? What happens when there’s a speech delay? What happens when you are medically complex as a preschooler?
00:30:12 Right? What happens in all these different times? And so it is for every parent, family and I say, and anyone who has a tiny human in their life. Right, because we discussed the range of issues. And so if you go to all the unexpected, which is one word, that is the hub.
00:30:35 There is links to the podcast, there to articles. We’ve produced two short documentaries this year talking specifically about black maternal health and the maternal mortality cris, which is deeply rooted in history. So as a historian, I’ve spoken about how we got here, and I think how we got here is a very important way to make change for the future. Because if you don’t understand how you’ve gotten somewhere, how do you move forward? Right?
00:31:05 Absolutely. We also have recipes for healthy living because I think nutrition is such a huge part of it, especially if you’re talking about preterm birth. Their gut, flora, their stomachs are incredibly, for lack of a better word, abused by the earliest parts of their lives. And so how do we nourish children, not only physically, but mentally and spiritually? So we talk about parenting.
00:31:35 Gentle parenting is a huge part of what we discuss. How do we evaluate our own emotions and our own emotional connections to children and sort of the things that they trigger in ourselves and kind of healing. And so it’s really about healing as a family, as a unit, as a larger community. So, like I said, anyone who interacts with the children. So, yeah, all the unexpected.com and also on all your friendly socials Instagram, facebook, Twitter, Discord, any of all of all.
00:32:13 The unexpected on all of the things. I love it. Yeah. That’s where you can find us. And I get comments and emails from I get comments and things from parents and it’s wonderful to hear from people all around the world.
00:32:30 So we’ve got podcast listeners in 64 countries right now. That’s amazing. I got an email from a mom in Nigeria saying, I heard my story in what you were talking about.
00:32:45 I love to hear from people. I have no problem answering questions or resources, and I find myself people will send me, hey, where can I find something about this? And I’m like, hold on and I’ll send you an email with ten links. Very much in the process of making sure that people have the resources they need and feel heard and feel seen. Well, there’s no doubt you’re doing that, and I’m so grateful that you came on Child Life On Call on call with me.
00:33:23 Well, thank you for having me. Yeah. Oh, my goodness, I would love to have you again at any time. So I hope that you do come back and continue to help us understand more about your experience, what you’re advocating for, so we can all continue to grow, feel less alone. And the healthcare professionals that listen to this can feel more connected and more empowered to do more, to really, like you said, not just facilitate, but deeply respect and understand that.
00:33:53 The way of the world for which it, quote, unquote, was supposed to happen is now turned around. So I really appreciate you. Thank you. And thank you for the work that you do. I think families are probably touched every day.
00:34:07 Thank you.
You Might Also Like…
216: How to talk with Kids about Child Abuse – Jane’s Story [Repost]
April is Child Abuse Prevention Awareness Month. We have reposted this episode to bring awareness and give you tangible tools to speak with your kids about child abuse. Today’s guest expert is Jane Donovan, who is a child abuse prevention advocate. "And like we say in...
215: Ruptured Appendix: Emergent Surgery, 6 Days in the Hospital & Struggles to Discharge
"I've learned so much in this whole process. It's like you have a depth inside of you that resurrects as an advocate and high alert, and it lives inside of you when you need it." -Aspen, Willa's Mom In this episode of Child Life On Call, host Katie Taylor and guest...