April is Child Abuse Prevention Awareness Month. We have reposted this episode to bring awareness and give you tangible tools to speak with your kids about child abuse. Today’s guest expert is Jane Donovan, who is a child abuse prevention advocate. "And like we say in...
Episode 181 | Jan’ s Story- A daughter with PVOD and Lung Transplant
Podcast Show Notes
Meeting Jan Stepps feels like catching up with a long-lost friend. Her warm demeanor and indomitable spirit immediately set the stage for impactful and reassuring conversations. A proud mother of two, Jan, is a resilient family figure who navigated an evocative journey through her daughter’s organ transplant process. Combining her personal experience with her daughter’s lung transplant and her knack for real conversation, Jan shares valuable insights on tackling the emotional roller-coaster that organ transplant journeys inherently become. Prior to this life-changing event, Jan was a confident career woman, expertly managing the role of a train dispatcher.
Organ transplants are life-changing procedures that touch the lives of countless individuals and their families around the world. They represent a beacon of hope for those living with life-threatening medical conditions, offering a second chance at life and healing. Understanding the transformative power of organ transplants is not only essential for those directly involved in the process but also for their families and support networks navigating this complex journey.
Here are the key steps:
- Understanding the Emotional Impact of Organ Transplants
- The Vital Role of Support Networks During Transplant Journeys
- Dealing with Feelings of Guilt in the Transplant Process
- The Positive Impact of Organ Transplants on Quality of Life
- Finding Strength and Resilience in the Midst of Medical Challenges
1. Understanding the Emotional Impact of Organ Transplants
I’ve had a thought-provoking conversation about the emotional impact of organ transplants, a matter that’s often overlooked amidst the clinical aspects of such procedures. The transformation isn’t only physical but also brings about a significant emotional shift in those affected. The process surrounds not just the patient but also engulfs their entire support system, marking it as an emotional congregation of hope, apprehension, and above all, resilience. The journey is convoluted, marked by anticipation, anxiety, and unfortunately, sometimes even grief. It’s an emotional rollercoaster from the moment the need for a transplant is realized, throughout the wait, and even post-transplant as the fear and bit of anticipation lingers on. Consider Jan Stepps, a mother who tread this path for her daughter, Jade. As Jan and her daughter navigated through the complex medical world of Pulmonary Veno-Occlusive Disease and lung transplants, they experienced the emotional turmoil often associated with organ transplantation. The waiting period, full of suspense and uncertainty, transformed their lives in extraordinary ways.
The strength Jade exhibits post-transplant, becoming a beacon of resilience in their family, and the fulfillment of her promise- the golden retriever at Christmas- depicts the powerful emotional bond and trust shared between them. For them, despite the hardships, it was essential not to lose sight of life’s joys. Jan’s candor about feeling anxious, the emphasis on trust, hope, and never giving up presents a realistic portrayal of the human side of organ transplants. However, the emotional impact of organ transplants and how it transforms lives transcends the medical world.
It reverberates on a societal level, shifting perspectives, and reshaping priorities drastically. It underscores the preciousness of life and the inherent human tenacity. It reinforces the notion of hope, even in the face of indubitable adversities, and the importance of holding onto the simple yet profound promises of life. Our narrative underlines the strength that blooms amidst the toughest circumstances and the remarkable bond it nurtures. It’s essential to remember that this journey doesn’t end at the hospital doors; rather, it extends beyond them, amalgamating into the very fabric of everyday life. And perhaps that’s why, to understand life and its essence, we must recognize and respect these emotions, as challenging as they may seem.
2. The Vital Role of Support Networks During Transplant Journeys
The role of support networks during transplant journeys is vital, whether that network is family, friends, or medical professionals who become an integral part of the process. Preparing for and undergoing an organ transplant is an intimidating and emotionally draining journey, one that requires both strength and resiliency. It’s a path filled with uncertainty, fear, and significant medical decision-making, all of which are made easier to bear with the solid foundation of a strong support team. A network of compassionate individuals can provide emotional welfare, physical necessities, and serve as sounding boards to discuss treatment options and outcomes.
This network’s presence allows for robust support in facing whatever medical or emotional challenges that may arise during this time. In retrospect, Jan Stepps reflects upon her journey and the significance the support network played during her daughter Jade’s lung transplant process. From the astute school teacher who first noticed Jade’s symptoms, her family physician friend who guided Jan to seek medical attention, to the parent support groups at the hospital, each individual played a crucial role in their journey. They helped Jan navigate the medical jargon, procedures, and emotional tumult associated with the transplant journey. Being four hours away from her support system, she relied heavily on the relationships built in the hospital, even though she felt hesitant about sharing her struggles. The shared experiences and camaraderie helped her feel less alone during her most vulnerable moments.
The importance of support networks during transplant journeys can’t be overstressed. They provide the emotional and mental strength needed to endure the stressful situations accompanying the process. By sharing their fears, hopes, and experiences, individuals navigating through similar situations feel a connection, a feeling of being understood without judgment – a sense of belonging.
This human connection is instrumental in maintaining emotional health, which is a crucial factor in managing physical health conditions. Traversing the path of organ transplant with a reliable network of support transforms the ordeal from an insurmountable challenge into a manageable process of healing and recovery. The journey might be arduous, but with mutual understanding and unwavering mental and emotional support, it becomes a shared journey towards hope, strength, and resilience.
3. Dealing with Feelings of Guilt in the Transplant Process
I remember the day my daughter, Jade, faced the daunting prospect of a lung transplant. It wasn’t easy for either of us. Jade was terrified of the procedure and I felt an overwhelming sense of guilt, constantly questioning if I was making the right decision for my child. As parents, we want to protect our children from any harm, and to make Jade face such a drastic procedure felt like I was betraying her trust. It was an emotional rollercoaster, filled with guilt and self-doubt. But at the end of it all, it was about making a tough decision that would ultimately save her life. Looking back, I can clearly recall how Jade would sob at the mere mention of a transplant. She was so young, yet she was forced to face such an adult decision.
Every time I pushed for her consent, it felt as if I was pushing her into a corner. There was a tight knot of guilt that gnawed at me. But Jade’s deteriorating condition was a stark reminder that this was our only option, our only chance at survival. Over time, Jade grew to understand this and while the fear never completely faded away, she bravely faced the situation. At the time, I didn’t realize that this guilt was a common feeling among parents navigating the organ transplant process. It’s impossible to shake off the responsibility we feel for our children.
We’re supposed to shield them from harm, not thrust them into it. But the harsh reality of life is that sometimes, there are no easy choices. There is only what is necessary. And while we can’t always protect our kids from life’s tough challenges, we can be there for them, every step of the way, providing unwavering support and unconditional love. And perhaps in doing so, we might find the strength to forgive ourselves and move past the guilt.
4. The Positive Impact of Organ Transplants on Quality of Life
In the vast and complex world of medicine, organ transplants represent a beacon of hope for many families afflicted with life-threatening conditions. These procedures offer not just a lifeline, but also an opportunity to dramatically transform the patient’s quality of life. From the exhilarating relief of finding a match to the grueling road of recovery, organ transplants are a tangible testament of modern medicine’s ability to make what was once thought impossible a reality. More than just a medical procedure, organ transplants also represent resilience, love, and above all, hope. It’s a profound journey that can bring about significant, positive change in the patient’s and their family’s life.
Take Jan Stepps for example. Her daughter, Jade, was diagnosed with Pulmonary Veno-Occlusive Disease, a frighteningly rare and severe condition that necessitated a lung transplant. Prior to the transplant, Jade was physically constrained by her illness, her every breath a struggle. Post-transplant, her world transformed: from the joy of welcoming a golden retriever into their family, a longstanding promise from Jan to Jade, to the exhilarating experience of participating in activities she could barely dream of engaging in before her health improved. The newfound freedom and independence that Jade enjoyed following her transplant displayed an inspiring testament to the capability of these intricate surgeries to impact the day-to-day lives of patients.
So, why does this all matter? Because every step taken, from diagnosis to recovery, matter to everyone involved and can fundamentally alter the course of their future. The transformation brought about by an organ transplant far equates the benefits to the physical improvements. It extends to psychological and emotional aspects, too. Patients like Jade, who have undergone an organ transplant, are likely to gain a newfound confidence, resilience, and overall zest for life. It injects hope into circumstances that once felt utterly hopeless, demonstrating the magnanimous effect such procedures can have on an individual’s quality of life.
Meanwhile, their families gain a renewed perspective on the intricacies of life, fostering resilience in facing challenges that come their way. In essence, the benefits and importance of organ transplants extend far beyond just physical healing. They’re transformative, providing a renewed lease on life, and a chance to embrace life with an inspiring strength and spirit.
5. Finding Strength and Resilience in the Midst of Medical Challenges
The transformative power of organ transplants is a profound narrative that signifies not just medical marvel but also an enduring human spirit. The journey towards an organ transplant often presents hefty challenges that demand strength and resilience. It is not just about the medical complications but also about the emotional vortex that engulfs families during the process. The real-life story of people who embark on this journey is a testament to human perseverance and the courage to face life-altering realities. Dealing with the diagnosis, grappling with consent, navigating through medical procedures, and living with the ever-present hope for a life-saving call – all of these form a mosaic of experiences that are both overwhelming and enlightening.
Coupled with the intense challenges are the instances of self-discovery and personal growth that open doors to a renewed appreciation of life. The journey of Jan Stepps, who navigated through her daughter Jade’s lung transplant, is a compelling example. Her experiences were marked with challenges ranging from getting Jade’s consent for the transplant to dealing with the distressing long-term hospitalization. These instances, while overwhelming, called upon a strength steeped in parental love. The strength to break down medical jargons for her daughter, the ability to keep Jade’s spirits up by fulfilling her wish for a golden retriever, and the unwavering option to stay resilient despite personal trials, underline her journey.
The narrative is not just about a medical breakthrough, but also about a journey characterized by continuous adaptation, resilience, and an undying hope for a brighter tomorrow. The journeys like those of Jan underline a profound realization about the significance of resilience during medical challenges. Such narratives underscore the human potential to face adversities head-on, adapt to unthinkable realities, and find strength from within. The stories are not just about surviving challenging times.
The transformative journey of organ transplant holds immense gravity for families navigating this path. The emotional complexities, the necessity of robust support systems, and the persistent feelings of guilt are facets of this experience that can be immensely challenging, yet are often overshadowed by the medical aspects. The inspiring stories shared here underscore the significance of these factors, pushing us to recognize and address them.
Moreover, they emphasize the remarkable improvement in the quality of life post-transplant, showcasing the resilience and strength that individuals and families often discover within themselves during these trials. As we move forward, let us carry these insights with us, fostering greater empathy, understanding, and support for everyone involved in such life-changing journeys.
Whether you are a parent or professional, we want you to join our community. Sign up for our newsletter here.
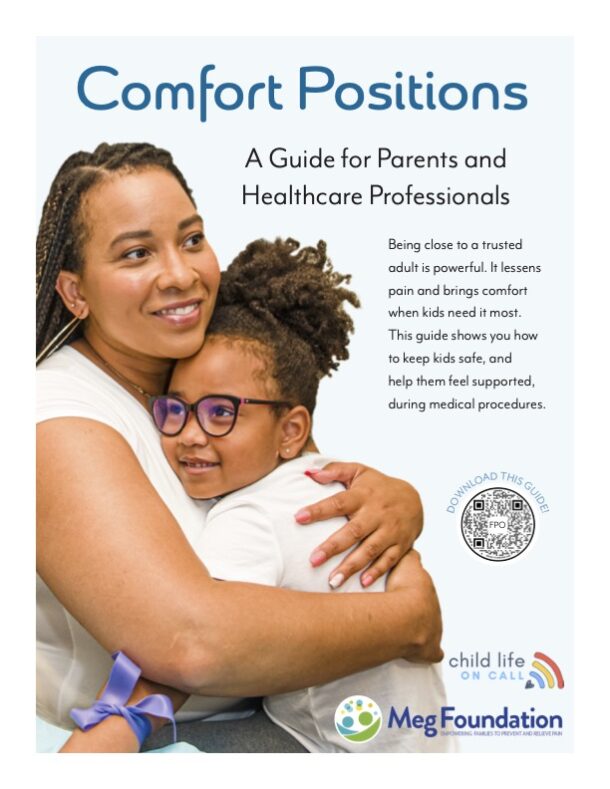
Parents, download our free parent starter kit.
When you download our starter kit, you’ll learn how to:
- Give medicine to your child without it becoming a wrestling match
- Prepare your child (and yourself) for a shot so they can feel less anxious
- Create and use a coping plan for any medical appointment or procedure
The first sign of sniffles, or worse, shouldn’t send you into a tailspin. Feel confident in your role as a parent and advocate, no matter what medical situation you’re facing.
Child life specialists, get affordable PDUs on-demand here.
Shop for your CLOC gear here.
Transcript:
00:00:00
You’re listening to episode 181 JM Story a daughter with PVOD and a lung transplant. Hello, my friends. Welcome to Child Life On Call. This podcast is a safe place for parents to share their stories about what it’s like to have a child that has a medical experience, diagnosis, disease, and or everything in between. We know there is power in sharing stories, and that power multiplies when you can listen to other parents who have walked a similar path to yours.
00:00:31
Giving and getting advice is great, but hearing how another parent navigates the complexities and nuances of healthcare is even better. As a child life specialist, my role is to support, validate, and provide emotionally safe spaces for kids and their families, and I am so honored to be on this journey with you. In addition to parent stories, we sprinkle in some expert episodes every now and again that have content for both parents and professionals in the field of healthcare, all with the mission to empower parents to be confident advocates and partners with the care team during healthcare experiences. We’re so glad you’re here. Hello, my friends.
00:01:09
I don’t know how I get so lucky to be able to do this job and host this podcast, because meeting people like Jan and hearing her tell her story is one of the biggest privileges I’ve had in my life. And that’s because Jan and her daughter have gone through something that is really unimaginable. And the reason she heard about this podcast was that she was on the same floor in an ICU as another mom who shared. And although their stories are so different, there’s a lot of similarities there between what they went through, and it’s not just because they were treated in the same hospital, but it’s because they both went through transplants, which is incredibly arduous situation. One of the most interesting parts of the story with Jan today was talking.
00:02:04
About how because her daughter was older. Her daughter needed to give consent or assent for the procedure to happen. And that’s not something I knew about or something I knew. I guess it’s something that I knew about. But I never really took into consideration how old a child has to be before they can give consent to a life saving procedure and how that can actually end up delaying sometimes the care that’s needed.
00:02:29
So I hope that you are able to take away some nuggets of wisdom and honesty that come from Jan’s story. It’s not always clean and simple. Sometimes it’s really messy and vulnerable. But Jan does an amazing job of describing the realities of being very new in this process, of having a daughter with a onset diagnosis of pulmonary hypertension, turning into PVOD and then a lung transplant. And as she says, her journey is still not over.
00:03:01
Well, I hope you enjoy this story and this conversation that I got to have with Jan, and I’m so grateful that you’re here with us. Today. We live in Fort Worth, Texas. I am married. It’s been five years.
00:03:13
We just celebrated our five year wedding anniversary. Congratulations. Thank you. Thank you. And we have Jade, who is now twelve, and her baby sister Jan, who is two and a half.
00:03:29
I was working full time right up until the morning of Jade’s diagnosis, and. I just have not been back to work since. Wow. What were you doing before her diagnosis? My husband and I both work for the railroad, so we were dispatchers.
00:03:44
Train dispatchers. Oh, my gosh, I’ve never met a train dispatcher. There should be a whole documentary film on what your job is. I’m sure they try to compare it to, like, air traffic control with planes, but just trains. Okay, got you.
00:04:01
Well, I know we’re going to be talking about your older daughter today. And you and I, before we just jumped on this, you were saying, like, we weren’t a medical family before all of this, and you just got kind of thrown into it. And I think that’s a really interesting perspective because a lot of the parents we have on the podcast either know, in utero or really early on. But it’s something else when your child has already lived a chunk of their lives and then something changes. So why don’t you walk us through kind of the very beginning steps of what happened?
00:04:33
Honestly, I thought Jade had asthma. That’s just the plain and simple of it. She would not really want to engage. In many sports or physical activities. But I thought, you know what?
00:04:47
I was athletic growing up. She just might not be. She might be like my artsy kid. I just thought she had asthma. She wouldn’t even come into, like, a grocery store with me.
00:04:57
Sometimes I’d even try to bribe her, like, hey, want to come into Target? Like, pick out a toy or something? No. She just seemed to slowly be withdrawing. A little bit more from any activity.
00:05:11
And so one day, one of her teachers called me and said, yeah, Jade told me she had asthma. Can you bring her inhaler up to school? Because she has to take some breaks just walking up the stairs. And I’m like, I talked to her doctor. Her doctor told me she did not have asthma.
00:05:28
And so that teacher had called me. Or maybe like a week, and my best friend, who is also a family physician, and our kids were in class together, she went up to field day at Jade’s school. And I had kind of been talking. To her about this stuff already, but she reached out to me and was like, I think you need to take her to get some blood work. Like, she keeps moving to the end of the line so she doesn’t have to participate.
00:05:57
And even when we walked a lap, she seemed kind of winded. So try to set something up with your doctor. I hope I’m not overstepping. I was like, no, not at all. I appreciate it because I’ve kind of been seeing some of this stuff.
00:06:11
And that was on a Friday. On the Monday was picture day. And she left school early. She started throwing up. So I called her doctor to try to get in for a sick visit.
00:06:22
And they saw us that Wednesday. So it’s just a couple of days. Between when she had told me that. And our doctor sent us for lab work and an x ray at the Child Life On Call hospital because she said she didn’t hear any of the wheezing that accompanies asthma. So we go down there, get an.
00:06:43
X ray, get blood work. The doctor calls me back later that afternoon and said the radiologist saw something. It might be nothing, but it was enough for them to suggest that we. Do a follow up with cardiology. All right, no problem.
00:06:59
I go the absolute next week. It was one week later, and they. Did an echo on her. And I just felt like while we. Were in the room, like something was wrong.
00:07:12
The tech said, all right, I’m going. To go ask the doctor if they need any more images. And I’m thinking, Well, I don’t think. That’S good if it was just a. Simple cut and dry and I don’t.
00:07:23
Know if we’d need extra images. So we go into the room with. The cardiologist and she was like, pulmonary hypertension. Her pulmonary artery is so enlarged. My nurses are already on the phone with the Child Life On Call hospital to make sure they have a bed for her.
00:07:40
So even her saying pulmonary hypertension, I. Wasn’T scared, not as much as I ended up becoming, but because I knew nothing about it. Nothing like, okay, I’m thinking, right, if it’s a condition, maybe some medicine and that’s that, we go from there. But then once we got down to. The Child Life On Call hospital, it kind of just became a whirlwind.
00:08:07
Like I felt like my head was on a swivel. They did a right heart catheter on. Her, and we were sitting in the waiting room. I remember it was my mother and. I and other doctors would come out.
00:08:22
And talk to the parents right there in the waiting room. Like, your child did great. And Jade’s doctor walked in and was. Like, okay, let me take you to. This room up here.
00:08:33
So I’m like, already red flags are. Going up, like consultation room. Like, if she was fine, everyone else. Got meetings right there in the waiting room. And.
00:08:54
That was the first time I heard lung transplant. And I’m thinking, I have an eleven year old child who is completely healthy. Like, you had to have gotten it wrong. Like, this.
00:09:09
Can’T be real life. I have recorded it, the conversation, because I wanted to be able to send. It to my friend so she could interpret. But it was just a lot of sobbing. Like they kept telling me her quality of life.
00:09:26
You kept saying, for the remainder of her life, and I’m like, Remainder of her life? Are you telling me it’s going to be cut short? I’m still not even fully comprehending what’s going that it kind of just started there. We ended up switching hospitals once we found out that Texas Child Life On Call was really the hospital we needed to be at. They were more equipped as far as.
00:09:53
Transplants and even their pulmonology department. So we transferred our care to them. And we got in with the pulmonologist there. She’s amazing. And she had told me on our.
00:10:09
First visit, which was on June 6. That the only thing that’s concerning me. Jan, is she’s on these medicines for PH, but she’s still needing her oxygen requirement. It hasn’t seemed to have gotten better yet. It’s actually kind of going in the opposite direction since going to the first Child Life On Call hospital.
00:10:30
And she said, I have a fear that it could be this Pdod, and. That would be the worst case scenario. And we went back home that day. So the difference between the two hospitals, they didn’t share the same system. So the Texas Child Life On Call doctor could not go in there and pull up the CT scan images or any of those test findings.
00:10:57
That first Hospital had to send them on a CD disc to her. So she called me back. Yeah, she called me back the next. Week, and it was after hours, so. I’m already like, all right, well, at this point, it’s just like one blow after the next.
00:11:16
There’s no calming down or chance to breathe or process or it’s it was just one thing after another. And she said, Are you in the room with Jade right now? I said no. She said, okay, good. I need to tell you, I would.
00:11:32
Bet my career on it that it is PVOD, and I need you to come down here. She said, I know it’s late in the evening. You guys live in Fort Worth, so first thing in the morning, I want you to head down here. She said, if it is PVOD, we could try to titrate some of her. Medicines, plan to be here for the weekend.
00:11:52
And before we get off the phone. She said, But, Jan, I want to. Be honest, I’m not sure how long you’ll be here.
00:12:00
So we were admitted to Texas Child Life On Call on June 16, and then we did. Not get to leave until October 10 of 2022. Yeah. Oh, my gosh. Yeah.
00:12:18
Oh, my goodness. I want to rewind a little bit because it’s just like you went from field day to lung transplant to long term chronic hospitalization, new diagnosis. And I’m sure looking back is incredibly emotional. I can see it in your face.
00:12:47
How did you handle that autopilot mode that you were kind of talking about? Like, unable to process, going step by step?
00:12:58
Did you have a sounding board like, I imagine your family physician friend was somebody you could text and say this. I can say just last night, I have a friend who’s an Er physician. Like, everybody needs a friend who’s a doctor, right? I’m like, can you look at this bump? And just somebody to process with.
00:13:18
Did your parents step up? Who did you find your community with during those initial phases? Or did you kind of keep it to yourself? How did you cope? I do think one thing that got.
00:13:32
Me through the hospitalization was how naive I was in the medical world. Because now I look back and I’m like, oh, my goodness. Those words from that echo mean heart failure. Like, I wasn’t really comprehending all of it, but yeah. So my best friend, she would be my sounding board, my sisters, my parents.
00:13:55
But at the same time, my sisters. And parents would also ask a lot of questions. And sometimes I didn’t even know. I don’t know. I’ll ask tomorrow or I’ll see.
00:14:05
It was very overwhelming for all of. Us because even within our family, our. Whole family, we haven’t had any issues like this. No one has ever been sick. So it was just a shock for everyone.
00:14:20
Everyone was supportive.
00:14:24
But it was like. A nightmare for all of us. It’s like walking the line of, like, how much information do I give without worrying them? But I also don’t want to have to answer this question because I don’t know it yet. It’s like a whole thing with even communicating with family members.
00:14:40
It is. And actually, I had seen something that talked about, like, a circle of grief, and I had to tell my family this. Jade and I are at the center. Who’S been like my sisters and my. Mom and dad and my husband and are in that next circle.
00:14:57
Like, everyone who is on the outer rings from the center of the circle. Does not release any of their stress. Or any of their drama that they’re going on in their life that maybe I would normally want to talk about. No, we can’t do that right now. I can’t handle it.
00:15:16
It needs to go outwards, keep that burden off of me, kind of visual. It’s such a powerful boundary that you have to set at the beginning because you just don’t have any room to process none. And you’re calling me about something that. Bothered you with a coworker. Okay, I think I got real issues right now.
00:15:39
We got some real stuff going on, some heavy stuff, but they were great about it. And once I expressed that, everyone kind. Of so that did help.
00:15:53
It’s a good lesson in stating what your needs are, even though these are difficult conversations. But when you’re in the mode that you are in, it’s just non negotiable. It has to be this way, and. I’m telling you yeah, sorry, not about you right now. We need some time.
00:16:09
Yeah. So going back to this weekend hospitalization that turned into months. How much of the information? Because Jade’s eleven. Right.
00:16:20
So she’s in the room, she’s hearing a lot of things. You’re both learning and processing at the same time. How did you guys handle telling her what was going on? And how did you notice her questions and how was that whole relationship?
00:16:38
This is the part that seems crazy. To me, is because she was eleven. They would not list her unless she agreed to the transplant. Every time the transplant team would come. Into the room, she would sob.
00:16:55
We couldn’t talk about the word transplant. She didn’t want to hear about it. It scared her, rightfully so. But then me as a mom, I’m. Like, we need to list her.
00:17:10
We don’t have a ton of time. Why are we waiting on her? At what point are you going to let me just be like, we’re doing this and list her, let’s go. They said eventually we would have gotten to that point, but we were admitted, like I said, June 16, and she was not listed till July 25. So it took about a month and a half for her to and she.
00:17:34
Never really even said, oh, I want this. She was like, I’m scared. I don’t want it, but I know. I need it in order to live. And to get out of the hospital.
00:17:44
So they accepted that from her as her willingness.
00:17:51
What age does that kind of consent going to? I don’t even know because she was only eleven at the time. But they said that obviously she was. Aware enough it was still her body. And they wanted to make sure that post transplant there would be compliance.
00:18:11
So they want the transplant to be successful as well. So they needed to make sure everyone was on board, the whole family. Will you explain to us a little bit about what PVOD is and what that diagnosis entails? So PVOD is pulmonary veno occlusive disease. It is the most rare and the most severe form of pulmonary hypertension.
00:18:40
And basically it’s like the veins within her lungs were like constricted, not completely obstructed, but her heart was not able to pump blood through her lungs because of how constricted they were. With that, the right heart goes into. Failure because now it’s working overtime to. Compensate for the lungs not functioning properly, doing their job.
00:19:16
The only treatment, it’s not even a cure, but the only treatment is a lung transplant.
00:19:27
And when you were in the hospital, we said you ended up meeting another family. Did you find any other families like yours?
00:19:40
Yes, there were two other families and. They were both like adolescent girls with PVOD. There were other children who needed lung transplants, but for like, cystic fibrosis or different diagnosis.
00:19:58
Yeah. So talk with us a little bit more about the process of transplant for you. And you’re kind of in this boat. It’s not like I want her to have a transplant, but she absolutely needs it to live. It’s the only thing we can do.
00:20:15
What kind of mode did you find yourself in when you were in that long term hospitalization and were you able to take breaks or how did you. Handle all of it? Oh, that is a loaded question. So.
00:20:33
Dealing with just the initial shock of transplant, the whole team came in. We had to do tons of meetings with every single different surgeon, dietitian. There were so many people that had. To basically give the okay, like, all. Right, this family will do what it takes.
00:20:57
And that was just so overwhelming. I remember we were there just maybe two or three days at that point and I got handed a binder, lung transplant binder. Read through this because we’re going to go over this and there’s a lot. Of information in there. Write down any questions you have.
00:21:16
But the team was great. They are amazing. So thorough. They really understood that this was so. Shocking and new to us.
00:21:28
There is part of me and it’s going to sound crazy to even vocalize it, but there is part of me that is envious of different organ transplant. Families because the lungs are the least successful.
00:21:46
I even sometimes get jealous like that, okay, you had a heart transplant, okay. But your stats aren’t as grim as. Mine or your child has a better chance. Even some families where their kids are. Born with a condition or they knew they had a whole life to I.
00:22:05
Don’T want to say prepare, but at least this is a possibility in our life. So I think it’s very difficult because. I think Jade and I still harbor some anger and bitterness. Like, why me? It was never even on our radar that she was sick.
00:22:26
And then it just comes out of nowhere and it’s so awful. And getting through the hospital stay was hard because I have a two and. A half year old and my husband still had to work to keep our insurance. So they stayed in Fort Worth and Jade and I are in the hospital in Houston. We don’t know anyone.
00:22:48
Three to 4 hours away? Yeah, 4 hours away. Not around our support system. She could not even leave her room because we were in ICU. So we were confined.
00:23:02
So a lot of times I even. Felt guilty walking down to get a coffee. She can’t leave the room. I wanted to do it in solidarity. With her because I felt bad.
00:23:17
I just wanted to be in it with her. So there would be times where my parents would come down, they would go and stay with her. I’d go grab dinner with my two and a half year old and husband once in a great while. I would not spend the night at the hospital. Someone else would spend the night with.
00:23:38
Her, but I would never leave her alone. I just would never do that. But I felt guilty taking breaks when she couldn’t. I think two of the things you’ve just expressed are incredibly courageous in my mind and very honest. And that is this kind of like you said, this grief and this anger and this bitterness around other people’s experience who may have a better chance.
00:24:06
Right. And why did they get that hand? And we got this one. And the second one is this feeling of guilt for leaving the room for any amount of time. And I’m sure you felt that when you did leave, there was like a sense of refreshment.
00:24:23
It’s like that shower, that life changing shower that you take that you can go in one person and come out another, but it doesn’t make it any easier to leave or take those moments for yourself. Well, and even every time I left, that would be the only time I would cry. I would never cry in front of. Jade about it because even before this. She was kind of anxious kid.
00:24:46
She feeds off me. So I’m not showing fear, I’m not showing worry. So that would be like, really, I would keep it bottled up and I leave for a couple of hours and now this is the only time I’m getting with Jan and my husband and I’m crying the whole done. It was difficult. Yeah.
00:25:07
Those other families that you got acquainted with, what were those relationships like? Were they helpful? I’m sure there’s also some sense of competition is probably the wrong word, but we’re all in this. We all need lung all, you know, going through this this camaraderie, but know, a little bit of jealousy for experiences. Jade has kind of had since her transplant.
00:25:34
She has caught COVID, got virus, broke her elbow. And I’m like, oh, I know. Just normal kid things. She was playing in the front yard.
00:25:46
So there are times where I’m like, they’re not having hiccups. Like, does this. And then I start going into all right, well, does this affect the longevity of how her lungs are going to do compared to their lungs? It is great to have some other. Moms that you can talk to that.
00:26:03
Get what you’re going through. But even then, I don’t want to. Reach out to her just when I’m going through it because she’s going through it too. So unloading these fears. All right, well, if she didn’t have.
00:26:17
Those fears, maybe now she’ll have them. If I’m vocal, it’s just really tricky. It is like a little community, like a little family. And you’re always cheering these other kids on. Yeah.
00:26:30
And I think that’s such a good perspective to consider because with families, it’s not all hunky dory all the time. You’re not always like, sharing your innermost thoughts, but you know your innermost thoughts with this other person. I find that really honest because sometimes we can have this idea I’m going to reach out to this other parent and they’re going to get it. But sometimes those relationships are tricky. Yeah, they are.
00:26:56
And it’s like you feel I deal. With a lot of guilt. You’ll pick up on that as we talk more. But I feel bad just going to another mom who I know if she. Feels anything like I feel, she’s already stressed.
00:27:13
I’m not trying to burden her with. Some of these things because I already know she probably is at her limit, too. So there is a sense of, you understand what I’m going through, and it is like a community. But on the same hand, I know I’m dealing with so much. Sometimes it’s overwhelming.
00:27:39
Yeah. And sometimes it’s hard to repeat. Like, I feel this way in therapy and even talking about what I do at work all day with my husband, somebody I trust so much, I’m like, I don’t want to relive what I just went through. I don’t want to talk about it again. It’s exhausting.
00:27:55
It’s emotional to have to think about all of it. So it’s just you have to balance the cost of talking about it and what that will emotionally tell you. And if the response isn’t what you want, it’s a whole bag. It is. Even now, when we go to certain doctors appointments, if it’s like a new doctor and they’re saying, all right, tell me what got you here, jade will.
00:28:16
Be like, Mom, I’ll talk. I don’t want you to cry again. I know. I feel so bad, but it is it’s just so sad and emotional and. It’S a lot what I hear is a preteen who knows what’s going on and has started to learn and advocate.
00:28:36
And I was talking with her name is Dr. Ina Taleb, and she’s Teen Health Doc on Instagram. I love her. She was on our podcast, and I was asking her about these kiddos who are preteen and adolescent with chronic complex conditions and how they transition into adult care. And she was like, they’re the best at it.
00:29:00
She’s like, they have been talking about it and hearing about it, and it was really great to hear her say that, that she finds that they really learn how to take care of themselves. I want to step back a little bit. So it’s the end of July almost. She says yes to the transplant, and then you go into transplant mode and tell us a little bit about that experience and moving forward. Yeah.
00:29:25
Even though we were inpatient. So it’s a little different because some. Kids are allowed to wait at home. They just have to be within a certain time frame of the hospital. But we were inpatient but phone on at all times.
00:29:38
Answer any phone call that comes through, because it could be the one. And actually, we had gotten I don’t. Want to say it was a dry run, but I had gotten a phone call after her being listed for, like. Five days we had gotten a phone. Call, it did not end up working out.
00:29:52
I think she was like second or. Third on the list. So they were not for her. Yeah, it was kind of anxious. I felt like I couldn’t see a light at the end of the tunnel.
00:30:07
We had been living in the hospital. I just wanted her to make it to get the transplant for her to. Be healthy enough to receive the transplant. So that was very nerve wracking. Every day that goes by, it’s just like, when is it our turn?
00:30:28
What were some of the things that helped her and you while you guys were in the hospital?
00:30:34
I will say, for me, I was given a gratitude journal from the palliative care team. I felt like that helped me. I had to come up with three. Things, so I would do it at nighttime and just write three things I was grateful for. And honestly, some days I had to.
00:30:54
Pick the most random thing because I had nothing. It was not a good day or I’m thankful I got a warm coffee this morning. Some days that was it that I felt helped me. I kept a journal, but I didn’t start writing in it until after her transplant. And I would just write her a letter every day.
00:31:22
I think one thing that really got. Us through the hospital stay, our child. Life specialists, Bailey and Adair.
00:31:34
I’m so grateful for them. I say that Bailey, like, single handedly. Got and Bailey’s a dog, by the way, canine therapy. But I say that they single handedly. Got her through that hospital stay.
00:31:49
There would be days she did not. Want any doctors to come in. Bailey was her one exception. So she would come once a week. But yeah, they’re amazing.
00:32:02
I never even thought of all these. Like, I was never in a hospital with her. I had no idea.
00:32:10
But I’m so grateful and so thankful.
00:32:16
We kept trying to make plans for. When we got out of the hospital. Let’s write a list, like, what do you want to do? What are things? Let’s give you motivation to want to get out of here.
00:32:28
And so one of the things she. Wanted was her own Bailey, her own golden retriever. So I have done my best. I’ve kept my word. She’s got her own golden retriever now.
00:32:42
Yeah, she got her for Christmas.
00:32:46
But I keep my word on those things because I felt like that was so important for her while we were there to not give up. And so these things that we have planned, we’re starting to do them and start living again. You talked about her hesitancy, which is completely honorable and understandable that she didn’t want to have to get a lung transplant. What eleven year old would?
00:33:20
Now that she has had the lung transplant, she’s on the other side. She’s getting her golden retriever. Life is not back to normal. Because there is no going back. Does she see why it was important and how bad she felt before, or it’s hard in a kind of young adolescent mind.
00:33:45
She does she’ll even make comments to me sometimes. We went to the water park the other day, for example. The last time we were there was about a week before her diagnosis, and my father had her on one of. These little rope course things in the water, and she didn’t even get halfway through it, and she started screaming, like, I can’t breathe. I can’t breathe.
00:34:12
Like, full panic mode. We just went, like, two weeks ago. And she looked at me and said, do you remember last time we were here? I couldn’t even do this. I couldn’t walk up the stairs to go on a slide.
00:34:27
I couldn’t do any of these things. I can breathe now. So now it’s just a matter of, like, PT, her legs feeling a little weak or something, but she’ll say, I can breathe. Yeah, she’s noticed a difference.
00:34:46
How does she handle the follow up visits? All that comes with, like, you talked about the team making sure that her compliance and your compliance, too. Right. You’re the one driving the ship, making sure meds get taken and that you get them, and she gets to appointments. It’s for sure a team.
00:35:04
How have you both been doing with.
00:35:09
We? We like, going back down to Houston. She gets to see her people. We stop in, and we see Bailey ands to. She doesn’t mind that part.
00:35:23
We do have local doctors that we see, like, in the interim, she’s not crazy about going to those appointments, but she doesn’t give me any pushback. She knows this is what we need. To do, and this is kind of. How life is right now, and as we get further out, those things will lessen. But, yeah, she looks forward to going.
00:35:47
Back down to Houston because we’ll also go to Galveston for a day, go to the beach. She loves the beach. So we just try to yeah, this. Is what we need to do, and. We just do it.
00:35:59
This is life now. Yeah. As we kind of get to the end of this episode, and I know it’s not the end of your story. But tell me about what you’ve learned about yourself since this. Onset, this diagnosis that this complete turning point of your life.
00:36:24
Like, what have you learned about yourself?
00:36:31
I don’t even it’s crazy because I still don’t feel like anything is about me. A lot of people will say, you’ve been through it, too, but I would. Trade positions with her in a heartbeat. Have no control over this. It just makes me think, and I verbalize it forward to friends, but I.
00:36:57
Thought I was stressed before diagnosis. In this day to day life, those things don’t matter. Once this happened, the only thing that mattered was keeping her alive, doing what we needed to do for her health. People always say, you’re so strong. I wish I was weak.
00:37:18
I wish I didn’t have to be strong.
00:37:22
I had no choice. None of us had a choice.
00:37:29
I used to think that I was a strong one. I think now she’s way stronger than me.
00:37:37
It makes just everything else seem so. Mindless and it really doesn’t matter in. The grand scheme of things we used to care about. I just don’t. It’s like that shift in perspective of what really matters.
00:37:52
You find that popping up in your everyday life still. I can imagine sitting at the traffic light and it just constantly follows you. It does. Because we’re still not even at that year mark post transplant. So I do feel like it’s very emotional still.
00:38:12
And I feel like I didn’t even process most of it until afterwards. Even just the other day I had. A breakdown about her transplant and what they were actually doing during that.
00:38:29
You yeah, it’s a lot. Yeah. Are there any other stories or parts of your experience that you were hoping to share that I didn’t ask you about? One thing is, I think Jade is so hilarious. You don’t have to use this if you don’t want to.
00:38:47
I want to hear all about her. I’ve been like chomping at the bit. She’s so funny. Like, she’s so witty. She has the best sense of humor.
00:38:56
And she was intubated for about a week after surgery because she is pretty anxious. They needed to make sure that she. Was really relaxing and staying calm. But when she woke up, she was still pretty loopy. And I had asked her, she said.
00:39:14
I had my transplant. And I said, yeah, you had it, it’s over. And I said, you want to know about your donor? Because I only had one fact about her. And she said, yeah.
00:39:26
I said, well, your lungs are from a girl. And she was 26. And without even skipping a beat, she. Said, so does this mean I can have a margarita? And I’m like, what in the world?
00:39:41
And so she has since named her lungs Margot and Rita.
00:39:49
Yes. She is so funny. Hilarious. I’m sure you’re ready for this beautiful moment and response. That is amazing.
00:40:02
I know. We were all dying laughing. She’s just so funny. So funny. So funny.
00:40:10
What shift in Jade have you seen?
00:40:14
I have seen she is a lot more trusting of herself now. I think before diagnosis, mom, I think very timid, maybe hesitant, and she kind of takes charge and trust, hey, this. Doesn’T feel right, or I don’t like this. And she’ll speak up for herself sometimes. I’m like, not so much.
00:40:41
But I really do feel like that. Kind of stubbornness really helped her through recovery. I love that we want these strong, opinionated little girls in our lives. Not a little girl anymore. She’s twelve years old.
00:41:00
My last question for you is why did you want to come on and share about what you guys have been through?
00:41:08
First of all, PVOD is so rare. I just think maybe having more awareness of the disease, even after her transplant. She had said to me, well, maybe now the doctors can study my lungs so other kids won’t get this to help other kids. She makes me cry so much with some of this stuff. She says, yeah, she’s so wise.
00:41:36
But also because I feel like this is partly healing for me too, being. Able to tell our story, what we’ve been through. I know, like, on my Instagram, I’ll. Make like, little videos, a lot of just some of the hospital stuff that we’ve been through. Maybe another mom is feeling the same way and just needs.
00:42:09
Some inspiration or so she doesn’t feel alone.
00:42:15
And I’ve told our coordinator that because. They put me in contact with a mom while we were in the hospital. And I would love like, she’s asked. Me before, and I have agreed to. It because it is very isolating and.
00:42:31
No matter how close your girlfriends are. Or your family, they don’t get it. They’re not the ones going through it. So I just feel like it’s really helpful to have someone who can remotely. Get what you’re going through and understand.
00:42:54
Well, there’s no doubt that you will and have done that and will continue to do that. And as much as we can share awareness about PVOD and signs and symptoms and treatment, we want to do that. I’m so grateful to you for coming on here and being really brave and saying hard things. And I want you to know that you deserve care as much as Jade does and to be taken care of and loved on and supported. My mom has always said since I was little, and it bothered me when I was little, but I get it now.
00:43:30
She was like, she’s going to kill. Me for saying this. She’s like, your heart is breaking and mine is breaking twice. It’s breaking for you and it’s breaking for me. And at first when I’m little, I’m like, you don’t know my pain.
00:43:46
But now I get it. It’s like we feel these things so deeply because our love runs so deep and it’s like the most beautiful but painful thing at times. So I just appreciate you being so honest about that. You’re through it. But as true transplant and most medical families know, there’s no end, right?
00:44:06
There’s just always what’s next? And sometimes it’s a little slower and sometimes it’s crisis. Yeah. And that is one thing too. I think a lot of people who don’t deal with transplants or even these.
00:44:21
Medical conditions, I think they assume, oh, she got a transplant, she’s fine. It’s perfect. It’s just getting started. Yeah, just the beginning. Thank you for being you.
00:44:34
And Jada’s so lucky to have you as her mom. And if people want to follow along with you and see some of those videos. Do you have a public social media, or how can people find you? I do. I made my Instagram public when we were inpatient.
00:44:49
We posted a lot about canine therapy. And I like to post a lot. About canine assistance because that is where Bailey did come from. And I just think they’re so important. And crucial to have in Child Life On Call hospitals because she not only was really there.
00:45:09
For Jade, we asked her to carry such heavy loads for us, and so. I try to bring even awareness for them, too. Wow. That’s another good question, is what resources do you recommend besides canine therapy or any PVOD groups that you think parents should join? So I am in a lung transplant group, a pulmonary hypertension group, because even.
00:45:39
Though she was transplanted, I feel like I could potentially be beneficial on that. Side of it, too, because she technically did have it. But art therapy, music therapy at Texas. Child Life On Call, they have video game therapy. How cool is get to he would.
00:45:59
Come in once a week, and they’d play video games for an hour, but I really never had any clue. Even Child Life On Call oh, my goodness. All of the activities and even because Jade would feel uncomfortable talking to me about some of her fears, the Child Life On Call specialists were amazing. She could talk to them, ask them questions. They brought in a doll with actual little plastic tubes coming out of them just so she could see, okay, when I wake up from my transplant, this is what to expect.
00:46:33
This is normal. We don’t need to freak out because she is pretty anxious, and they were wonderful. Do you think that helped her? Because that’s always a question we get. If your child runs anxious, does seeing it make it scarier or does it help?
00:46:52
What do you think? Typically, I would say it would make. It scarier for her. However, I think she needed to see it. She was at an age where she.
00:47:03
Was aware even child life would tell. Me she’s asking me questions that my. Older teens ask me. What happens if I wake up during surgery? What happened?
00:47:15
So they were really great in being. Honest with her, but they did know she was anxious, so they eased into it. It took a lot of time for her to have those conversations. Yeah, that’s true. It’s not always like, come in, sit down here’s what’s happening.
00:47:39
Bye. It’s sometimes building that confidence that you. Can learn about it. Yeah. Well, what is your social media so that everybody can come follow you?
00:47:50
My Instagram. It is Jan Ashley with two E’s. Ten. Jan ashley ten. Awesome.
00:47:57
Well, I will make sure to tag you, and I’m so grateful to get to meet you. I’ll actually be in the Dallas Fort Worth area this weekend for the we’ll send. There’s going to be so many dogs there. I’m so excited. Oh, my goodness.
00:48:13
But thank you so much for coming on here and being with me. Thank you for having me. Thank you all so much for listening to Child Life On Call. If you head to our website, Child Life On Calloncall.com, you’re going to find all sorts of. Stuff there for parents, professionals, healthcare providers, Child Life On Call specialists, no matter who you are.
00:48:34
Actually, when you just go to our homepage, it’ll tell you. It’ll help you direct to exactly where you need to go. On that, you’ll find opportunities and PDUs for child life specialists, parents. We’ve got a starter kit for you. And clinicians.
00:48:47
We even have a clinician course which teaches you how to be a confident and capable caregiver in pediatrics. We’re so grateful that you’re here. Please DM us on instagram. And like I mentioned, you rate and review this podcast. It helps other families be able to find us.
00:49:03
So let’s keep doing that and I will see you again here next week.
You Might Also Like…
215: Ruptured Appendix: Emergent Surgery, 6 Days in the Hospital & Struggles to Discharge
"I've learned so much in this whole process. It's like you have a depth inside of you that resurrects as an advocate and high alert, and it lives inside of you when you need it." -Aspen, Willa's Mom In this episode of Child Life On Call, host Katie Taylor and guest...
214: Sacrifice, Advocacy, Joy: Raising a Son with End Stage Kidney Disease – The Ransome Family’s Story
"Sometimes it's really therapeutic though to remember all that you have gone through because I feel like there are times when we look at each other and I'm like how did we get here?" Taylor Ransome We're grateful for our sponsor for this episode, Nestle Health...