April is Child Abuse Prevention Awareness Month. We have reposted this episode to bring awareness and give you tangible tools to speak with your kids about child abuse. Today’s guest expert is Jane Donovan, who is a child abuse prevention advocate. "And like we say in...
Episode 183 | An EMS professional shares how to prepare your child for an ambulance ride
Podcast Show Notes
In the world of emergency medicine, there is an unexpected twist that few are prepared for. It’s a twist that involves children, their fears, and the daunting task of medical transportation. But one man, Josh Itano, has discovered a way to unravel this twist and bring comfort to both parents and their little ones. His journey, from fascination to insight, has led him to a revelation that could change the way we prepare children for ambulance rides and hospital transfers. Brace yourself, for the key to unlocking this twist, lies in understanding the unique needs of these young souls…
Being present, validating, and really listening to kids and families is the magic potion to building a connection and earning their trust. – Josh Itano
My special guest is Josh Itano
Introducing Josh Itano, your guide to understanding the nuances of having your child in an ambulance ride or hospital transfer. With around three and a half years of practice in Emergency Medical Services (EMS), Josh’s experience ranges from working in suburban settings to lending his expertise in more rugged, wilderness conditions. Currently a volunteer with the Glenwood Volunteer Fire Department, he shares not just his knowledge of the field, but his passion for better connecting with patients of all ages. Josh proves that even in the most distressing circumstances, understanding the experience from a child’s perspective can help ease fears and anxieties.
This is Josh Itano’s story:
Josh Itano had always harbored a fascination for the field of emergency medicine, drawn to the blend of unpredictability and purpose. The adrenaline rush, the satisfaction of making an immediate impact, and the ability to alleviate distress in critical moments were all part of his allure. But there was another aspect that intrigued him: the interaction with children and families. The delicate task of explaining the unfamiliar, the daunting, and the often scary to a child. The first realization of this interest came when he noticed the shock registered on the faces of EMS trainees learning about child life specialists’ role for the first time. It prompted Josh to explore further, to try and bridge a gap he saw between EMS and child life specialists. His curiosity ultimately led him to a valuable insight: children are not just mini adults. Their needs, their understanding, and their coping mechanisms are unique, and understanding this makes all the difference.
In this episode, you will be able to:
- Delve into the intertwined nature of Child Life and EMS, highlighting their integrative importance in emergency medical scenarios.
- Learn about the power of family involvement and effective communication during critical times.
- Gain insights into strategic ways to prepare children for ambulance travels and hospital shifts.
- Discern the role of visual aids and boon of preparation books in calming children during hospital transfers.
- Understand the necessity of building open and supportive spaces for pediatric patients.
Being transparent and communicative is so crucial when engaging with children during an ambulance ride or hospital transfer. Pediatric patients can feel uncertain about this new and unexpected journey, making them apprehensive. Being honest with them about what to expect can ease this worry and establish trust. Let them know it will be filled with various people, flashing lights may be on, and sirens might sound. Always remember, children appreciate honesty and respond positively to it.
Josh Itano’s perspective brought a lot of depth to this topic. He spoke about the need to get detailed information from the patient, such as their medical history and allergies. But I’m sure Josh would agree, it’s not just about asking questions, it’s about taking the initiative to explain what’s happening. As Josh suggested, painting a real-time picture of the situation for kids can make them feel involved and can alleviate their anxiousness.
Here’s the thing about children – they need our attention and empathy. This is especially important when they are being transported for medical reasons. It’s critical to validate their feelings and listen to their concerns throughout their medical journey, acting as their confidant. By doing so, we help to create a safe space for them to express their worries and fears.
Katie Taylor echoed this sentiment during her talk with Josh. She spoke about how Child Life Specialists focus on being present, validating, and attentive to pediatric patients. She strongly believes in providing children with the space to express themselves and letting them know it’s okay to remain silent if they wish to. As Katie emphasizes, every child is unique and may require a different approach, but they all need someone to listen to them attentively during such critical times.
Creating a sense of familiarity during medical transport can do wonders in reducing a child’s anxiety. Imagine, being a child, having a team of unfamiliar faces rush in with urgency – it surely can feel intimidating, right? So to help alleviate the situation, we need to find ways to introduce some comfort elements. This could come in the form of trauma teddies, perhaps a favorite blanket or a soothing song. It’s about trying to bridge the gap between the unfamiliar (ambulance) and the familiar (home). Pediatric psychology points to such strategies as instrumental in reducing stress and tension during high-stress moments.
Well, didn’t Josh Itano make a nice point about this aspect? He mentioned how vital it is to be conscious of the child’s feelings during an ambulance ride. When Josh discussed about how some ambulances carry trauma teddies, it got my mind racing to how these fuzzy toys might just be enough to create a distraction and add a pleasant element to an unfamiliar surrounding. A potentially alarming situation can certainly become a smidge more manageable with these small yet thoughtful considerations.
The resources mentioned in this episode are:
- Follow Child Life On Call on social media for updates and resources for parents and professionals in the healthcare field.
- Consider becoming a Child Life On Call specialist to provide support and emotional safe spaces for kids and their families during medical experiences.
- Connect with Josh Itano on LinkedIn to learn more about his experience as an EMS professional
- Explore the Child Life On Call website for more information and resources on how to prepare your child for an ambulance ride.
- Check out the Child Life On Call podcast for parent stories, expert episodes, and advice on advocating for your child during healthcare experiences.
- Consider donating to or volunteering with organizations like Wilderness Medics and other EMS services to support their important work in emergency medicine.
- Practice deep breathing and calming techniques to help your child stay calm during an ambulance ride and provide
Whether you are a parent or professional, we want you to join our community. Sign up for our newsletter here.
Parents, download our free parent starter kit.
When you download our starter kit, you’ll learn how to:
- Give medicine to your child without it becoming a wrestling match
- Prepare your child (and yourself) for a shot so they can feel less anxious
- Create and use a coping plan for any medical appointment or procedure
The first sign of sniffles, or worse, shouldn’t send you into a tailspin. Feel confident in your role as a parent and advocate, no matter what medical situation you’re facing.
Child life specialists, get affordable PDUs on-demand here.
Shop for your CLOC gear here.
Feel empowered with Child Life On Call’s Mastering Immunizations: Expert Tips to Prepare, support and respond like a Child Life Specialist Course for Parents, Child Life Specialists, and Clinicians! 🌈👨👩👧👦💉
It is the only course you’ll ever need to be able to prepare, respond and support your child at any age and stage for immunizations. Evidenced-based tips from a child life specialist who has been supporting kids through painful procedures for 13+ years. This offer will only be available for a limited time. Pre-order your course today here!
Podcast Transcript
00:00:00
You’re listening to episode 183. An EMS Professional tells us how to prepare your child for an ambulance ride.
00:00:11
Hello my friends. Welcome to child life on call. This podcast is a safe place for parents to share their stories about what it’s like to have a child that has a medical experience, diagnosis, disease, and or everything in between. Queen we know there is power in sharing stories, and that power multiplies when you can listen to other parents who have walked a similar path to yours. Giving and getting advice is great, but hearing how another parent navigates the complexities and nuances of healthcare is even better.
00:00:40
As a Child Life On Call, my role is to support, validate, and provide emotionally safe spaces for kids and their families, and I am so honored to be on this journey with you. In addition to parent stories, we sprinkle in some expert episodes every now and again that have content for both parents and professionals in the field of healthcare, all with the mission to empower parents to be confident advocates and partners with the care team during healthcare experiences. We’re so glad you’re here. Hello my friends. I’m so happy that you’re joining us today for this really special episode.
00:01:15
In my career as a Child Life On Call specialist, whenever I was working in with the Er, we always had the chance to work with the ambulance drivers and then EMS professionals who literally serve families during their most traumatic times in their home and bringing them to places and can handle crises like no other. So it was amazing when Josh reached out to me as Child Life On Call and said, how can I get better at my job? And I thought, how can we get. Better at our job? So today’s conversation is kind of a two way street.
00:01:45
He prepares us for what kids and families can experience when it comes to ambulance rides or if you or your child has gone through one, it might be really refreshing to hear this is exactly what is supposed to happen. And then we talk a little bit about, from a child life perspective, how EMS professionals and those who are working in the field, in families homes, or in ambulance rides can really make a difference for families and kids. So I’m so excited to share this episode with you. Let’s get started. My name is Josh Itano.
00:02:17
I’ve been a practicing EMT basic for about three and a half years now. So by not necessarily new, but not experienced by any means. So I’ve worked private EMS back in the suburbs of Chicago, and I served as eMTB Field Training officer and chaplain there. I’ve also worked for Wilderness Medics on what’s called their REMS team. And then I currently am volunteering with the Glenwood Volunteer Fire Department, fire department responses as well as EMS.
00:02:47
Wow. I’m so interested. What made you want to get into emergency and medicine and kind of this helping career that you’ve chosen sure. Absolutely. So that’s a little bit of a hard question.
00:03:01
It kind of goes back to before I can remember. So I used to live back in Chicago, and we lived right by a hospital, so every once in a while, we’d have fire tars go by, so I’d run over, put on all my gear, but that was all way before I could remember. So honestly, it couldn’t really quite answer it just because it was so long ago. I kind of fell into EMS as a default because I was originally wanting to go into fire, and then EMS is kind of part of fire. Okay.
00:03:33
Are your family members in a position like yours? No. No one’s in EMS fire, anything like that. Wow. It’s one of those things that’s like a calling.
00:03:43
And I think a lot of us as Child Life On Calls, too, it’s like, as soon as you realize that that’s what you want to do, that’s just what you go for. 100%. Well, you and I have kind of just been connecting over email for a bit, but what made you want to reach out and talk more about not only Child Life On Calls, but kind of the integration between child life and EMS? And I know from my experience working in an Er, a lot of times EMS trainees would come through, and we would work with them and kind of teach them about what we do with kids. And it’s usually a shock, like, oh, my gosh, you guys exist, and how do we get you into ambulances and all of this stuff?
00:04:23
And I’m just so appreciative of all that you do and how you serve, but I’d love to know your interest in kids, families, and kind of that connection where you were drawn to reach out. Sure. Absolutely. So I became aware of Child Life On Call specialists through Facebook post, and after realizing there was such a thing as a Child Life On Call, I was like, oh, because I’ve never heard of that before in all my years of working. And we get training, obviously, in pediatrics, how to handle newborns all the way up to someone passing away.
00:04:58
But generally, kids are healthy in modern societies compared to some older folks. And so while we get the train in it, we don’t necessarily always am 100% comfortable with interacting with pediatrics. And I can speak from my own personal experience that I’ve interacted multiple different times with kids, but it’s never been, like, kind of second nature with talking to eight year old, 60, whatever going on down. Yeah, it’s that whole, like, working with adults is one thing, but kids are not many adults, and you probably realize that. Absolutely.
00:05:37
I’m kind of curious. What have you found that has worked for you in your experiences? Maybe from your first interaction with the family to your later interactions? What have you found? When you do something, it tends to work better.
00:05:50
Sure. Absolutely. So most of the time when I’m working with someone, it is patients that are probably wanting to hurt themselves and it’ll be taking them from a hospital to a behavioral health hospital. So a lot of the times just being upfront and honest with them and also obviously involving the family members having their buy in is huge. And most of the time that’s worked pretty well for me.
00:06:15
I know when you get to a little bit younger kids, I’m kind of like what you guys deal with a lot. With Child Life On Call specialists, you go five and below. That’s where it’s a little bit more difficult for me and where I haven’t had as much exposure. Yeah, that’s incredible because first of all, you’ve picked up on two of the biggest things that we use as Child Life On Calls. One is honest preparation for what to expect, and second is including the family system.
00:06:42
So you’ve literally already picked up on two of our biggest skills that we try to do, and especially with you picked up that adolescent population that we do see in the hospital and is very real and prevalent now in our society. And like you said, people just adolescents especially, just want you to be honest with them about what to expect and where you’re going to take them and how long it’s going to take to get there. And I think one of the things we try to do as Child Life On Calls is help them handle what is happening in that moment. It doesn’t matter what brought them here. It does matter what brought them here.
00:07:19
But really just with respect and saying right now, here are some things that you can do to get through this moment right now, and I’m a safe person to help you do that, and I’m going to make sure you know exactly what’s going to happen next so we can get through that moment too. Have you found that? Yes, most definitely. And another thing that I forgot to mention a little bit earlier is depending on what is happening, obviously it’s very situational dependent. But what has worked for me very well is not necessarily always talking, but being willing to listen, let’s say 89% of the time.
00:07:56
And then just letting the conversation naturally evolve from that point, I’ve definitely found has also been very helpful. Yeah, it’s like there’s no need to fill that space with us being an expert and having to talk at them, but like you said, just being willing to listen. And then I think a lot of people are like, Child Life On Call, what’s the magic potion? What’s the sauce that you use to get families or kids or adolescents to talk with you? And a lot of times it’s just being present validating and being really quiet and willing to listen.
00:08:31
And probably on those rides, you have some time, right, to just listen. And I know a lot of times that’s like a real luxury that we get in our career is time. A lot of times we’re doing it as fast as possible. Yes, most definitely. And there’s been times where you got to go, go.
00:08:49
And there’s other times where you might be taking someone from a very small hospital all the way out to, let’s say, city of Chicago. So you might have an hour’s span of time where you can really listen to someone and kind of get their. Know and talking with parents in my career clinically. And then on the podcast, they remember those rides. You’ll almost always hear about a transfer and the ambulance came and how that’s such a critical part of their story because it’s so different than anything they’ve ever experienced.
00:09:20
So I imagine if I were to get on an ambulance and I met someone like you who is just so calm and compassionate, it would be just a wonderful experience. So thank you for giving off the vibe that I’m already getting from you. All part of the job, but it’s all good. So I know that you came with a few questions about working with kids and what questions do you have? And I think you did mention the five and under one, and we can kind of talk through that, but is anything else coming up for you?
00:09:52
So, really one of the big things that I’ve found, especially with patients that want to hurt themselves, is that it’s very difficult to get them open up. And I’m sure you’ve had experiences with this, parents have had experience with this, and so where they’re just kind of going through a difficult time, I would most definitely feel the same way as they are. But any specific experiences you’ve had with helping kids get open to you or anything like that, I definitely appreciate, of course. So, yeah, let’s start with that one. We really try, and I’m sure you do too, to respect kind of the boundaries within our profession and that we’re not licensed psychologists or psychiatrists or counselors.
00:10:37
And we really try to make the patients know that right up front. So that is not my role. My role is for right now, to help you get through this. But I found what works the most is literally just being there and validating and just honoring that their experience, they may want to talk about it and they may not, and sometimes I do. Just say those words like, you do not have to open up to me.
00:11:03
You and I have the next hour together, and because we’re on this ride, I want to let you know I’m here to listen. But I’m not going to force you to say anything. Just know I’m a safe space. One thing I will do is check in every ten or 15 minutes because that’s part of my job. I have to take your blood pressure or this or whatever that may be, and I might ask how you’re doing, and you don’t have to answer if you don’t want to.
00:11:26
And sometimes it just takes the pressure off the kiddo to feel like they have to speak to an adult about something or that something they say is going to put them in, quote, unquote, more trouble or cause more harm to their family. So really putting that up out front as soon as possible I found is really helpful. Have you found that too? Absolutely, yes. And really, just like you said, being outfront and honest.
00:11:53
Whether it’s someone like, let’s say you’re bringing a kid for a trauma transfer, obviously that for those of you who don’t know, it can be either. All hands on. Deck because someone’s really having problems. Or it could be it’s a kind of precaution, but just like, preparing the kids and the families that, hey, there’s going to be a lot of people in the room, or something like that. Or introducing the kids to the nurses, doctors or whatever.
00:12:23
Yeah. And I found like even going pretty detailed can help with the conversation. Get going and have them ask questions. So you’re going to see the nurses and doctors wearing hats. They’ll likely all be wearing the color blue because that’s what this hospital wears.
00:12:37
Everybody in the hospital has a different color. So it’s almost like you’re being a source of comfort and information and so that when they do need someone to come or open up to, they’re looking to you because they know you’re going to give you detailed insight that they normally wouldn’t. One of the things we tried to do in our hospital, I know other Child Life On Call specialists, has too, is a preparation book of pictures so that they know exactly what the ambulance ride is going to be like and what the transfer hospital is going to be like. Can you walk us through what an ambulance ride is like? So let’s say it’s obviously a non trauma, right?
00:13:15
So the patient is awake and talking. Can their caregivers be with them? What is going to be happening to them when they’re in the truck? So a lot of it kind of depends. Starting off with can caregivers be in the truck?
00:13:30
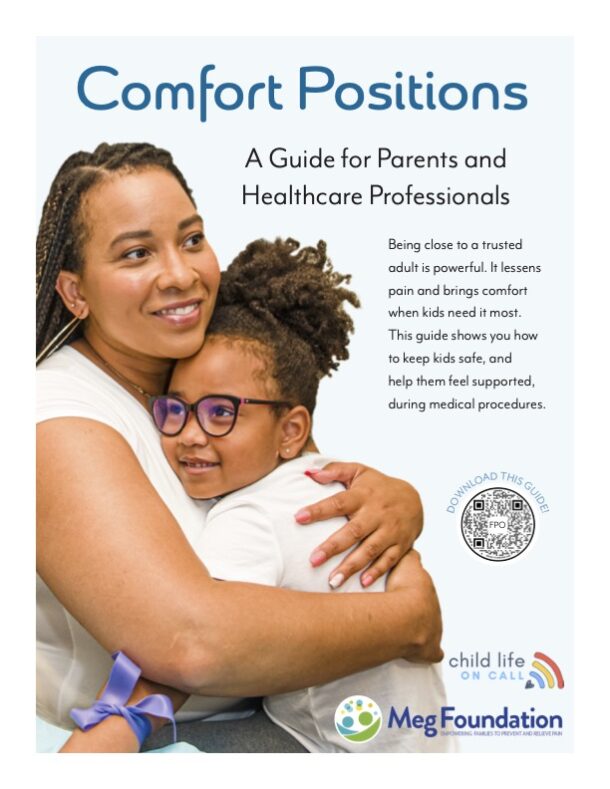
That’s a lot of times dictated by the times we’re in and our policies. So like, for example, during COVID it was no parents with the kids unless they are really sick and we need them to make potentially last minute decisions, in which case then, yes, we would make an exception. At other times it can be based on what the provider is comfortable with. So one thing that I’ve seen parents do a phenomenal job with is if they’re able to take a deep breath and just settle down and they’re helping the kids calm down, that is perfect. That’s exactly the kind of parent, and I’m sure you have experience with this too, that I would love to have in the back knee, especially if a kid is very worried.
00:14:17
So getting back to your question. Can the parents ride in the back knee? Amos or the siblings or whatever? It depends on where you’re at, what time. As far as doing either an inter facility transport or an IV, one, what most often happens is we will show up.
00:14:37
Depending on how serious the call sounds like dispatch. We may either send just two people or it may be a whole bunch of people. From that point, we will start getting a lot of information from you. So information like your full name, date of birth, if you have any medications, past medical history, allergies, anything like that, or any other questions. At the same time, one or multiple people will be working on taking vitals.
00:15:05
So blood pressure, your pulse. And then depending on the area, I’m getting what’s called a blood glucose level. So there’s this little what we call lancet, and I’ll stick your finger real fast and I’ll pinch for just a second. That’ll draw a little bit of blood, but that’s so we can make sure that you have enough sugar in your body.
00:15:26
From that point, if you’re very seriously sick, we’ll take your vitals again every five minutes or so. Sometimes it gets a little bit chaotic in the back of the ambulance. If you’re not so sick and you’re kind of just let’s say I fell and let’s say my shoulder hurts or something like that, and you said medical call, or my stomach hurts. Let’s just go with that. At that point, we’ll be monitoring you about every 15 seconds, taking that blood pressure again, checking to make sure, hey, are you all good?
00:15:57
Nothing’s changing? All right, perfect. So that’s kind of how it runs. Probably about five to ten minutes before we get to the hospital, we’ll do what’s called an inbound report. So it’ll be either on a telephone or on the radio.
00:16:12
And that’s when we’re just calling the hospital to give them a heads up to say, hey, here’s what we’re bringing in. Just let you know. And depending on how busy they are and a couple of other factors, the nurses in the Er will either tell us to go to the waiting room or to go straight to a bed or go to a trauma room occasionally. And this probably wouldn’t happen with an adult or pediatric patients. They may potentially take us straight up to surgery or something like that, or the catheter.
00:16:46
That’s so helpful to know. Thank you so much. So really, I hope what parents and professionals who work with kids are hearing is it’s almost like a mini doctor visit ride, right? So there’s an inbound report, there’s an outbound report, you’re meeting new people, you’re getting your vital signs taken. It just all happens in an ambulance.
00:17:07
Yes, exactly. And one thing that I think that parents really could help set this stage well is if you can say, hey, here’s what’s going to happen. So let’s say you have to take vitals, all that kind of stuff. There’s going to be a lot of people in the room. If your kid’s already kind of nervous in this and emergency situation, which is understandable, I would definitely feel the same way if you could just prepare your child to say, hey, there’s going to probably be a lot of people coming in.
00:17:34
There’s going to be a fire truck, ambulance, lots of flashing lights, but they’re all here to help you. Or just kind of prepare them somehow for what exactly is going to happen, which I’m sure you’ve done multiple times before in the hospital. Yeah, that’s really helpful. And here’s a silly, stupid question. Are the sirens as loud inside the vehicle as they are outside?
00:17:56
So if a child has some sensory issues, is that something they need to prepare? For sure. It kind of depends on how far away from the ambulance you’re standing. So obviously, if you’re right next to the siren, it’s going to be massively loud. Generally in the back of the ambulance, you can still carry on a fairly normal conversation.
00:18:17
You don’t really have to be shouting, but there’s also other factors that can play into it. Like, let’s say if you’re going down a gravel road, obviously it’s going to be pretty bouncy. Let’s say you’re in City of Chicago where you got skyscrapers all around. The sound is going to reflect that, but you can pretty much always I can’t recall a single time where I had to shout or yell. Just carry on a normal conversation.
00:18:41
That’s really helpful and good to know because I know sometimes it’s alarming when you’re outside of it and it’s so overwhelming, but when you’re inside you’re able to have a normal conversation.
00:18:52
I’d love to go back to kind of that younger kiddo age group and some of the things that I’ve found that has really helped them. And if you have questions or insight, I would love to hear them. So one is involving the parent as much as possible. They have already been in their life in a stressful situation with their child. So I like the parent to tell me what happens normally when they’re upset.
00:19:16
Like, what do you do to help them calm? And then that way they say, well, they love this song or they like to hold this blanket, or they like to do this or that. So you’re pulling on things or coping skills that have already worked before and how can we integrate that? The second thing I like to do is really normalize what they’re going through, although it is anything but normal. For instance, even when I am preparing a child for an IV that they’ve never had before, they certainly use soap to wash their hands every single day.
00:19:50
So I talk about how, you know, how you use soap at home. We have the same soap here, except it comes on a little white square. It feels cold and wet just like your soap at home. So taking some of those abnormal things, getting an IV, is not normal, but actually soap is pretty normal or vice versa. Like, your car has bright red lights on it, but you only have two, and this car has so many.
00:20:14
So although what they’re going through is different and something they’re not used to, you can really pull on their experiences as just being a human and what they do every single day and integrate that. Absolutely. And that brought up one point that I hadn’t thought of. So it’s not always the case with every single ambulance and every single fire truck, but at some departments, like the one I’m on right now, we have what are called trauma teddies. So, like little stuffed bears that every once in a while we can give the kid.
00:20:47
And if you want to ask for it, hands down, if we have it, we’ll definitely give you one. But that’s one thing that a lot of people might not be familiar with, but a lot of ambulance I’ve seen has the traumatins. What do you notice that does for kids when they get it? I’ve actually have not been able to give it to one because when I was back in Chicago, a lot of our trucks didn’t wind up having it. And when I’m out here, I’m still pretty new, so I actually haven’t had any experience with giving it to kids.
00:21:16
Yeah. So some of the things I noticed, because we do similar things in the hospital, one is it immediately becomes this non threatening item. Right. They have something that is not going to hurt, touch them, and then I try to use it whenever possible as part of their coping plan. So when we are looking at your arm or your hand, your job is to squeeze Teddy as hard as possible, right.
00:21:39
Or can we look at Teddy’s arm first and then we’ll look at your arm? So just kind of it’s almost playful, you know, and making it not only a comfort item, but really using it to help prepare the child can be really helpful. Absolutely. And that definitely be, like you said, really helpful. Because, I mean, in the ambulance I went over vitals, the transport that kind of runs, but obviously we’re also hopefully getting IV.
00:22:04
If you’re a sick patient, there’s a couple of other interventions that might have to happen, but an IV is definitely the most common. And so being able to say, can you just squeeze it on? The pay would be smooth. Yeah. I also love the idea of especially if the child isn’t too sick and able to respond and you can say, have you ever played I Spy in an ambulance before?
00:22:27
Let’s start. And just making it really playful. And then maybe when they remember that experience, they’ll look back and say, I got to play I spy in an ambulance. And even if kids don’t want to play because they don’t feel well, right? If their belly hurts, if they broke their arm, you can play it with yourself.
00:22:47
And I know that sounds silly, but being like, I spy something gray, what do you think it is? So just getting kind of in the mind of a child. A lot of times kids are too sick when they’re in an ambulance or a hospital, but playing next to them is almost as good as them playing when they’re not feeling up to it. Sure. Absolutely.
00:23:08
No, that’s a phenomenal idea. I’ll definitely have to try that my. Next it definitely feels silly the first time, right? But then it’s like the idea of taking a glove and blowing it up and making it into a balloon animal. You’re playing for them, playing next to them.
00:23:24
And these are tried and true tricks. Yeah, sure. Absolutely. No, that’s a great suggestion right there. Well, you talked so much about how parents play such an important role.
00:23:35
Are there any other insights or piece of advice that you would like to give parents who are listening? So this kind of tags along with my make no mistake that if your kid is very sick, it is okay to step outside, take a second, breathe if you need to sit here or whatever, that is perfectly fine. I’ve seen a while ago you’re taking this one kid, and he was a young kid, about ten or something like that, and so we load him in the ambulance, and I could see his mom was struggling as I loaded him in. She said goodbye, and then she walked around the side of the ambulance and she spoke right there. The real important thing was that she was there for her kid, and she is still a human, and it is perfectly okay to cry, but she was there.
00:24:31
And I thought that was phenomenal. Then, just like I said, preparing your kid for what’s going to happen. So maybe they might have to have an IV, maybe not. There’s some other interventions that might be necessary, depending on what it is that might not be comfortable. But just preparing, saying, hey, here’s what you can pretty much guaranteed.
00:24:52
We’re going to take your vitals, we’re going to call hospital, there’s going to be a lot of people, lots of flushing. So just kind of preparing them for that. Yeah, I think those two points are beautiful. It’s not that you want to hide your feelings from your child, but you never want them to feel like they’re taking care of you in that scenario, or that you’re so heightened that they’re feeding off of it. That doesn’t mean that those feelings can’t exist, but there might be a time and place where you can get support for then.
00:25:24
You know, like you said, it’s like a doctor’s office on wheels and prepare your child for what that experience could be like, and saying, I don’t know, we’ll find out. Together or you’re going to find out with my new friend Josh, I trust. And and those kind of things would be really great. Well, thank you so much for joining us and giving us so much helpful information about ambulance rides and some things I never even thought of or considered before and so grateful for people like you doing the job that you do and taking time to educate us and just really grateful for you. Absolutely.
00:26:03
Yeah, it’s my pleasure, for sure. Thanks so much. And we got through the episode without the sirens going off. It’s a win. Thank you all so much for listening to Child Life On Call.
00:26:15
If you head to our website, Child Life On Calloncall.com, you’re going to find all sorts of stuff there for parents, professionals, healthcare providers, Child Life On Call specialists, no matter who you are, actually, when you just go to our homepage, it’ll tell you. It’ll help you direct to exactly where you need to go on that you’ll find opportunities and PDUs for Child Life On Call specialists parents. We’ve got a starter kit for you and clinicians. We even have a clinician course which teaches you how to be a confident and capable caregiver in pediatrics. We’re so grateful that you’re here.
00:26:47
Please DM us on instagram. And like I mentioned, when you rate and review this podcast, it helps other families be able to find us. So let’s keep doing that and I will see you again here next week.
You Might Also Like…
215: Ruptured Appendix: Emergent Surgery, 6 Days in the Hospital & Struggles to Discharge
"I've learned so much in this whole process. It's like you have a depth inside of you that resurrects as an advocate and high alert, and it lives inside of you when you need it." -Aspen, Willa's Mom In this episode of Child Life On Call, host Katie Taylor and guest...
214: Sacrifice, Advocacy, Joy: Raising a Son with End Stage Kidney Disease – The Ransome Family’s Story
"Sometimes it's really therapeutic though to remember all that you have gone through because I feel like there are times when we look at each other and I'm like how did we get here?" Taylor Ransome We're grateful for our sponsor for this episode, Nestle Health...